Unlocking the Potential of Weight Loss Injections: A Modern Medical Perspective
In the evolving landscape of obesity management, weight loss injections and injectables have emerged as powerful tools that blend medical innovation with personalized care. Unlike traditional diet plans, these treatments offer targeted biochemical pathways to suppress appetite, enhance metabolism, and promote sustainable fat loss. However, their effective application demands an expert understanding of both benefits and risks, ensuring patients achieve lasting results without compromising health.
Beyond the Needle: How Weight Loss Injectables Transform Fat Loss
Injectable medications, such as GLP-1 receptor agonists, leverage the body’s natural hormonal signals to regulate hunger and glucose metabolism. This approach not only fosters significant weight reduction but often improves associated metabolic conditions like type 2 diabetes and hypertension. For example, semaglutide and tirzepatide, FDA-approved in recent years, have demonstrated remarkable efficacy by modulating appetite centers in the brain, reducing caloric intake, and enhancing insulin sensitivity.
These advances represent a paradigm shift from purely behavioral interventions toward medically guided therapies that address obesity as a chronic disease. Yet, success hinges on integrating these injectables into comprehensive, doctor-prescribed weight loss plans tailored to individual physiology and lifestyle factors, as detailed in expert medical guidance.
Injectables in Action: Real-World Insights and Patient Experiences
Consider the case of a middle-aged patient with obesity and prediabetes who initiated semaglutide injections under medical supervision. Over six months, alongside modest dietary adjustments, they experienced a 15% reduction in body weight and marked improvement in glycemic control. This illustrates how injectable therapies can act synergistically with lifestyle changes to yield clinically meaningful outcomes.
What Are the Primary Risks Associated with Weight Loss Injections?
Despite their promise, weight loss injectables are not without risks. Common side effects include gastrointestinal discomfort, nausea, and in rare cases, pancreatitis or gallbladder disease. Moreover, patient adherence can be challenged by injection-related anxiety or cost considerations. It is crucial that these treatments be administered within a framework of thorough medical evaluation and ongoing monitoring to mitigate adverse effects and optimize safety.
Choosing the Right Injectable: Navigating Options with Clinical Expertise
With an expanding array of FDA-approved injectables available, selecting the best option requires careful consideration of efficacy, safety profile, patient comorbidities, and personal preferences. For instance, semaglutide offers robust weight loss but may not be suitable for individuals with certain gastrointestinal disorders. Exploring these nuances in consultation with healthcare providers ensures personalized, evidence-based care.
For further detailed comparisons, readers may consult comprehensive resources such as the semaglutide vs. tirzepatide analysis, which elucidate differences in mechanism and outcomes.
The Future of Weight Loss Injectables: Integrating Innovation with Patient-Centered Care
Ongoing clinical trials continue to refine injectable formulations, aiming for enhanced efficacy with reduced side effects. As telemedicine expands access, patients worldwide can receive tailored treatment plans, combining cutting-edge pharmacotherapy with lifestyle coaching. This integrative approach underscores the necessity of expert medical oversight to harness the full benefits of injectables safely.
To explore how telemedicine simplifies access to these therapies, consider reviewing key benefits of telemedicine in weight loss treatment.
Curious about whether injectable weight loss treatments could suit your journey? Share your thoughts below or explore our comprehensive guide to choosing the best options in 2025.
For authoritative insights on the medical efficacy and safety of GLP-1 receptor agonists in obesity management, the New England Journal of Medicine review offers a rigorous scientific foundation.
Personal Reflections on Overcoming Injection Anxiety and Staying Consistent
When I first started with weight loss injections, I was honestly intimidated by the idea of self-administering shots. The thought of needles was enough to make me hesitant, and I worried about sticking with the regimen long term. But what helped me was breaking down the process into manageable steps and focusing on the ultimate goal instead of the momentary discomfort.
For example, I created a small ritual—preparing my injection kit in a calm space, using relaxation techniques before and after, and tracking my progress visually. These little habits made the injections feel less daunting and more like a daily act of self-care. Over time, the initial anxiety faded, replaced by a sense of accomplishment every time I saw positive changes in my health.
How Do Lifestyle Changes Complement Injectable Treatments?
One question I often hear from friends and readers is, “Can I rely solely on weight loss injections, or do I still need to change my diet and exercise?” From my experience and medical guidance, injections work best as part of a holistic approach. They help regulate appetite and metabolism, but sustainable fat loss also depends on balanced nutrition and physical activity.
Incorporating moderate exercise and mindful eating not only amplifies the effectiveness of injectables but also builds habits that support long-term health. For instance, when my doctor prescribed semaglutide, I paired it with simple lifestyle tweaks like increasing my daily steps and choosing whole foods over processed snacks. This synergy accelerated my progress and improved my energy levels.
What Are Some Practical Tips for Staying Motivated Through Medical Weight Loss?
Staying motivated can be challenging, especially when weight loss plateaus or side effects emerge. Here are some practical strategies that have helped me and many others:
- Set realistic, incremental goals to celebrate small wins.
- Keep a journal to track how your body responds and how you feel emotionally.
- Join support groups or online communities to share experiences and advice.
- Maintain regular check-ins with your healthcare provider to adjust your plan as needed.
Such approaches reinforce accountability and provide emotional encouragement, which is vital during any medical weight loss journey.
The Role of Trustworthy Information in Making Informed Decisions
With so much information online, it’s easy to feel overwhelmed or misled. I’ve leaned heavily on credible sources like the New England Journal of Medicine and trusted medical websites to understand the science behind injectables and their risks and benefits. This confidence in my knowledge helped me engage more meaningfully with my doctor and tailor a plan that suited my unique needs.
For those considering weight loss injections, I recommend exploring comprehensive resources such as doctor-prescribed weight loss plans and the detailed comparisons in semaglutide vs. tirzepatide to make informed choices that align with your health goals.
Have You Experienced the Intersection of Medical Treatment and Lifestyle Change?
Every journey is personal and unique, and I’m curious—how have you balanced medical treatments like injections with lifestyle changes? Have you found particular strategies or support systems invaluable in your progress? I invite you to share your stories or questions in the comments below. Your insights might just inspire someone else navigating a similar path.
And if you’re just starting, don’t hesitate to explore our comprehensive guide to weight loss injections in 2025 or reach out through our contact page for personalized advice.
Decoding the Pharmacodynamics: How Weight Loss Injectables Interact with Human Metabolism on a Molecular Level
Understanding the intricate mechanisms by which injectable weight loss therapies exert their effects is essential for clinicians and patients seeking optimal outcomes. GLP-1 receptor agonists, such as semaglutide and tirzepatide, act by mimicking endogenous incretins that enhance glucose-dependent insulin secretion while delaying gastric emptying. This dual action not only suppresses appetite but also improves postprandial glycemic control, thereby addressing two critical facets of metabolic syndrome simultaneously.
Emerging research indicates that these agents may also influence central nervous system pathways beyond the hypothalamus, modulating reward circuits linked to food intake and hedonic eating behaviors. This neuroendocrine modulation suggests a complex interplay between peripheral and central signals that could explain variable patient responses and necessitates personalized dosing strategies.
How Do Genetic Variations Affect Individual Responses to Weight Loss Injectables?
Pharmacogenomics increasingly reveals that genetic polymorphisms in receptors, enzymes, and transporters relevant to GLP-1 analogues can significantly impact efficacy and tolerability. For example, variations in the GLP1R gene may alter receptor binding affinity, influencing therapeutic outcomes and side effect profiles. Understanding these genetic factors can empower clinicians to tailor injectable treatments, potentially through companion diagnostic testing, enhancing precision medicine approaches in obesity care.
Such insights are crucial, as highlighted in a recent publication by Frontiers in Endocrinology, which underscores the role of genetics in modulating GLP-1 receptor agonist responses.
Integrating Behavioral Economics and Patient Psychology to Overcome Adherence Barriers
Beyond pharmacology, the success of injectable weight loss regimens heavily relies on patients’ psychological readiness and sustained adherence. Behavioral economics principles can inform strategies to nudge patients toward consistent injection routines and lifestyle modifications. For instance, implementing loss aversion tactics by framing adherence as a way to avoid health deterioration rather than solely achieving weight loss can motivate sustained engagement.
Moreover, cognitive-behavioral therapy (CBT) adjuncts tailored to injection anxiety and lifestyle adjustment challenges can address emotional barriers. This holistic approach recognizes that injection anxiety is not merely a physical hurdle but is intertwined with the patient’s mental frameworks and social environment.
Combining Injectable Therapies: Exploring Synergistic Potential and Clinical Considerations
While monotherapy with GLP-1 receptor agonists remains standard, the frontier of obesity pharmacotherapy is exploring combination injectable regimens to maximize efficacy. For example, co-administration of GLP-1 analogues with amylin mimetics or GIP agonists promises synergistic effects on appetite suppression and energy expenditure.
However, these combinations raise complex clinical questions regarding cumulative side effects, pharmacokinetic interactions, and patient selection criteria. Rigorous clinical trials are underway to delineate safety profiles and identify biomarkers predictive of favorable responses to polypharmacy in weight management.
Clinicians must weigh these factors carefully, balancing innovation with patient safety, to optimize individualized treatment plans.
What Are the Long-Term Implications of Chronic Weight Loss Injectable Use on Metabolic and Cardiovascular Health?
Longitudinal studies are essential to elucidate the enduring impacts of sustained injectable use. Preliminary data suggest improvements in cardiovascular risk markers, including reductions in blood pressure, LDL cholesterol, and inflammatory cytokines, contributing to decreased atherosclerotic progression. However, concerns about pancreatic health, potential nutrient malabsorption, and neuropsychiatric effects necessitate vigilant surveillance.
Healthcare providers should implement comprehensive monitoring protocols encompassing metabolic panels, cardiac assessments, and mental health evaluations to ensure holistic patient well-being over extended treatment durations.
For professionals and patients seeking to deepen their understanding of these complex dynamics, consulting specialized resources and engaging in multidisciplinary consultations can significantly enhance treatment outcomes.
Decoding Genetic Influences on Injectable Weight Loss Efficacy
Recent advances in pharmacogenomics have illuminated how individual genetic variations profoundly modulate responses to weight loss injections. Polymorphisms in genes such as GLP1R not only affect receptor binding affinity but also influence downstream signaling pathways, thereby altering appetite suppression and metabolic benefits. Recognizing these genetic determinants allows clinicians to customize treatment regimens, minimizing adverse effects while maximizing therapeutic outcomes. This precision approach is particularly valuable given the heterogeneous patient responses observed in clinical practice.
How Can Pharmacogenomics Personalize Injectable Weight Loss Therapy?
Pharmacogenomic profiling offers a roadmap to anticipate patient-specific responsiveness to GLP-1 receptor agonists and related compounds. By identifying biomarkers predictive of efficacy and tolerability, healthcare providers can select optimal agents and dosing schedules tailored to genetic backgrounds. This strategy enhances adherence and mitigates risks, paving the way for truly individualized obesity management.
For an in-depth exploration of this cutting-edge field, the Frontiers in Endocrinology publication on GLP-1 pharmacogenomics provides comprehensive scientific insight.
Harnessing Behavioral Economics to Enhance Patient Adherence and Outcomes
Incorporating principles from behavioral economics can revolutionize adherence strategies for injectable regimens. Techniques such as framing treatment benefits in terms of loss aversion and employing commitment devices effectively counteract injection-related anxiety and motivational decline. Additionally, integrating cognitive-behavioral therapy components addresses psychological barriers, fostering sustained engagement with both pharmacotherapy and lifestyle modifications.
Exploring Synergistic Combinations: The Next Frontier in Injectable Obesity Treatments
Emerging research investigates the potential of combining GLP-1 receptor agonists with agents like amylin mimetics and GIP agonists to achieve amplified appetite suppression and metabolic enhancement. These combination therapies hold promise for overcoming the plateau effect often encountered in monotherapy, although they necessitate careful clinical monitoring for cumulative side effects and pharmacokinetic interactions.
What Are the Long-Term Metabolic and Cardiovascular Implications of Continuous Weight Loss Injectable Use?
Longitudinal data increasingly suggest that chronic administration of weight loss injectables contributes to sustained improvements in cardiovascular risk factors, including reductions in blood pressure, LDL cholesterol, and systemic inflammation. However, potential concerns remain regarding pancreatic safety, nutrient absorption, and neuropsychiatric sequelae. Comprehensive patient monitoring protocols encompassing metabolic, cardiac, and mental health parameters are imperative to safeguard long-term well-being.
Clinicians and patients aiming to navigate these complexities are encouraged to consult multidisciplinary expert teams and authoritative resources to optimize treatment trajectories.
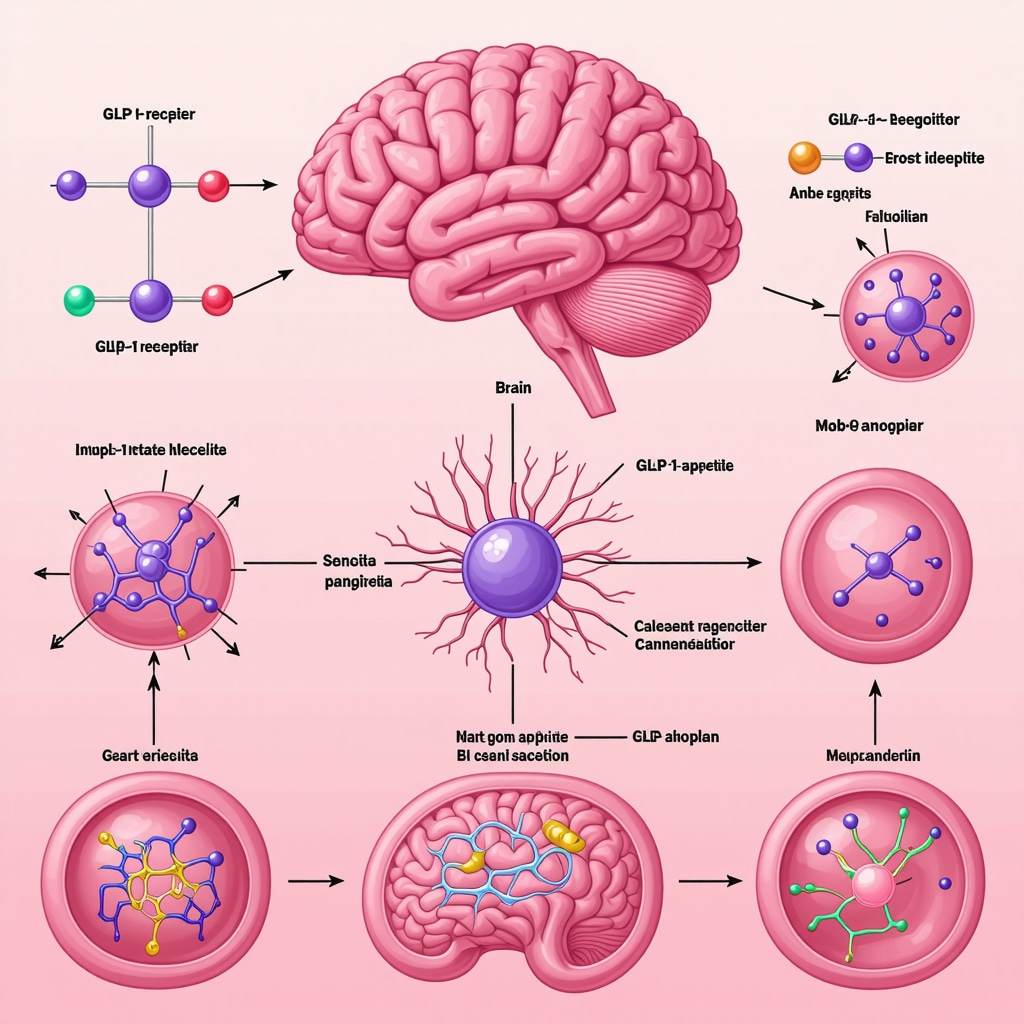
Unlocking Visual Understanding: Mechanistic Pathways of Injectable Weight Loss Agents
The molecular interplay between GLP-1 receptor agonists and central appetite regulation involves intricate signaling cascades affecting both peripheral glucose metabolism and central reward circuits. Visualizing these pathways enhances comprehension and facilitates patient education, promoting informed consent and adherence.
Ready to elevate your understanding and clinical approach to injectable weight loss therapies? Connect with our experts and explore personalized strategies tailored to your unique metabolic profile.
Frequently Asked Questions (FAQ)
What are weight loss injections and how do they work?
Weight loss injections are medically prescribed injectable therapies, primarily GLP-1 receptor agonists like semaglutide and tirzepatide, that mimic natural hormones to regulate appetite, delay gastric emptying, and improve insulin sensitivity. They reduce caloric intake and enhance metabolism, facilitating sustainable fat loss and improved metabolic health.
Are weight loss injections safe for everyone?
While generally safe under medical supervision, weight loss injections may not be suitable for individuals with certain gastrointestinal disorders, pancreatitis history, or specific allergies. Side effects such as nausea and injection site reactions are common. A thorough medical evaluation is essential to determine individual suitability and ensure safety.
Do I need lifestyle changes alongside injections?
Yes. Injectable therapies work best when combined with balanced nutrition and regular physical activity. These lifestyle modifications complement the pharmacological effects, promoting long-term weight maintenance and overall health improvement.
How long does it take to see results from weight loss injections?
Patients typically observe weight loss within weeks, with significant changes often evident after 3 to 6 months of consistent use alongside lifestyle adjustments. Individual responses vary based on genetics, adherence, and baseline health.
Can genetic factors influence my response to injectable treatments?
Absolutely. Genetic polymorphisms, particularly in the GLP1R gene, can affect receptor binding and metabolism of the drug, impacting both efficacy and side effect profiles. Pharmacogenomic testing may eventually guide personalized treatment choices for optimal outcomes.
What are the common side effects and how can they be managed?
Common side effects include gastrointestinal discomfort, nausea, and occasional injection site irritation. These often diminish over time. Strategies such as dose titration, dietary adjustments, and behavioral support can help manage symptoms effectively.
Is there a risk of long-term complications with continuous injectable use?
Long-term data suggest benefits in cardiovascular risk reduction and metabolic control; however, continuous monitoring is required to watch for potential pancreatic issues, nutrient absorption problems, or neuropsychiatric effects. Regular follow-up with healthcare providers is crucial.
Can I combine different injectable therapies for weight loss?
Research is exploring combination therapies, such as GLP-1 receptor agonists with amylin mimetics or GIP agonists, to enhance efficacy. However, these combinations require careful clinical oversight to manage potential side effects and interactions.
How can behavioral strategies improve adherence to injection regimens?
Incorporating behavioral economics principles like loss aversion framing, commitment devices, and cognitive-behavioral therapy can address injection anxiety and motivation challenges, fostering consistent adherence and better long-term outcomes.
Where can I find reliable information to make informed decisions about weight loss injections?
Consulting peer-reviewed journals, authoritative medical institutions, and healthcare professionals is essential. Resources such as the New England Journal of Medicine and specialized endocrinology publications provide scientifically vetted information to guide treatment decisions.
Trusted External Sources
- New England Journal of Medicine (NEJM): Offers comprehensive, peer-reviewed reviews and clinical trial data on GLP-1 receptor agonists and obesity pharmacotherapy, supporting evidence-based medical decisions.
- Frontiers in Endocrinology: Provides in-depth research on pharmacogenomics and mechanisms underlying injectable therapies, advancing personalized medicine in obesity treatment.
- American Diabetes Association (ADA): Features guidelines and position statements on metabolic management including injectable agents impacting weight and glycemic control.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Supplies authoritative data on obesity pathophysiology and emerging therapeutic strategies, enhancing patient and clinician education.
- ClinicalTrials.gov: A resource for tracking ongoing and completed clinical trials investigating the safety and efficacy of weight loss injectables and combination therapies.
Conclusion
Weight loss injections represent a transformative advancement in obesity management, bridging molecular pharmacology with personalized patient care. By leveraging GLP-1 receptor agonists and emerging combination therapies, these injections offer targeted appetite regulation and metabolic enhancement that surpass traditional interventions. The integration of pharmacogenomics and behavioral strategies further refines treatment efficacy and adherence, ensuring nuanced, patient-centered approaches.
Nevertheless, the success of injectable weight loss regimens depends on comprehensive medical oversight, lifestyle optimization, and vigilant long-term monitoring to maximize benefits while minimizing risks. As clinical evidence evolves, so too will the sophistication of these therapies, promising improved outcomes for individuals confronting obesity.
Empower your weight loss journey by engaging with trusted medical professionals, exploring evidence-based resources, and embracing holistic strategies that combine cutting-edge injectables with sustainable lifestyle changes. Share your experiences, ask questions, and continue learning to unlock the full potential of these innovative treatments.

What I find most compelling about weight loss injections like semaglutide and tirzepatide is how they signify a shift towards treating obesity as a complex, chronic disease rather than just a matter of willpower or diet fads. The way these injectables work by influencing the hormonal and neural pathways that regulate hunger and metabolism really highlights the sophistication of modern medicine. That said, the post rightly emphasizes that these treatments aren’t standalone magic bullets. From my understanding and experience, coupling injectables with lifestyle changes such as mindful eating and regular physical activity is crucial for long-term success.
Additionally, the discussion about the role of genetics in individual responses to these drugs is fascinating. It makes me wonder how soon pharmacogenomic testing will become a routine part of obesity treatment, enabling truly personalized care. On the flip side, I’m curious about how behavioral challenges, like injection anxiety and adherence, might affect outcomes and what innovative support strategies might help patients overcome these barriers.
For those who have tried or are considering weight loss injections, how have you balanced the medical treatment with lifestyle modifications? Have you noticed differences in results based on your approach? Sharing such insights could really enrich the community’s understanding and support.
This post sheds light on the rapidly evolving field of injectable weight loss therapies, which I find both promising and complex. A personal observation from my friends dealing with obesity is that adherence remains a significant barrier, especially when starting injections. The psychological aspect, including injection anxiety and motivation, often seems underrated despite the medical advancements. I recently read about integrating behavioral support and technology, like reminder apps, to improve compliance.
What intrigues me is the potential for genetic testing to personalize treatments further. As pharmacogenomics advances, do you think it will become standard practice before prescribing these injections? The idea of customizing doses based on genetic makeup could revolutionize outcomes.
Also, considering the cost and accessibility, how do we ensure these cutting-edge therapies reach underserved populations without widening disparities? Would love to hear any strategies or thoughts on making these treatments more equitable while maintaining safety and efficacy.