Unlocking the Potential of Prescription Weight Loss Pills: A Modern Medical Perspective
In an era where obesity and weight-related health issues are escalating globally, the demand for safe and effective weight loss solutions has never been greater. Prescription pills designed to assist in weight management have emerged as a scientifically backed option for many seeking sustainable fat loss beyond traditional diet and exercise. However, understanding which medications truly deliver results with minimal risks requires navigating a complex landscape of drug types, mechanisms, and clinical evidence.
Beyond the Basics: Exploring the Science Behind Prescription Weight Loss Medications
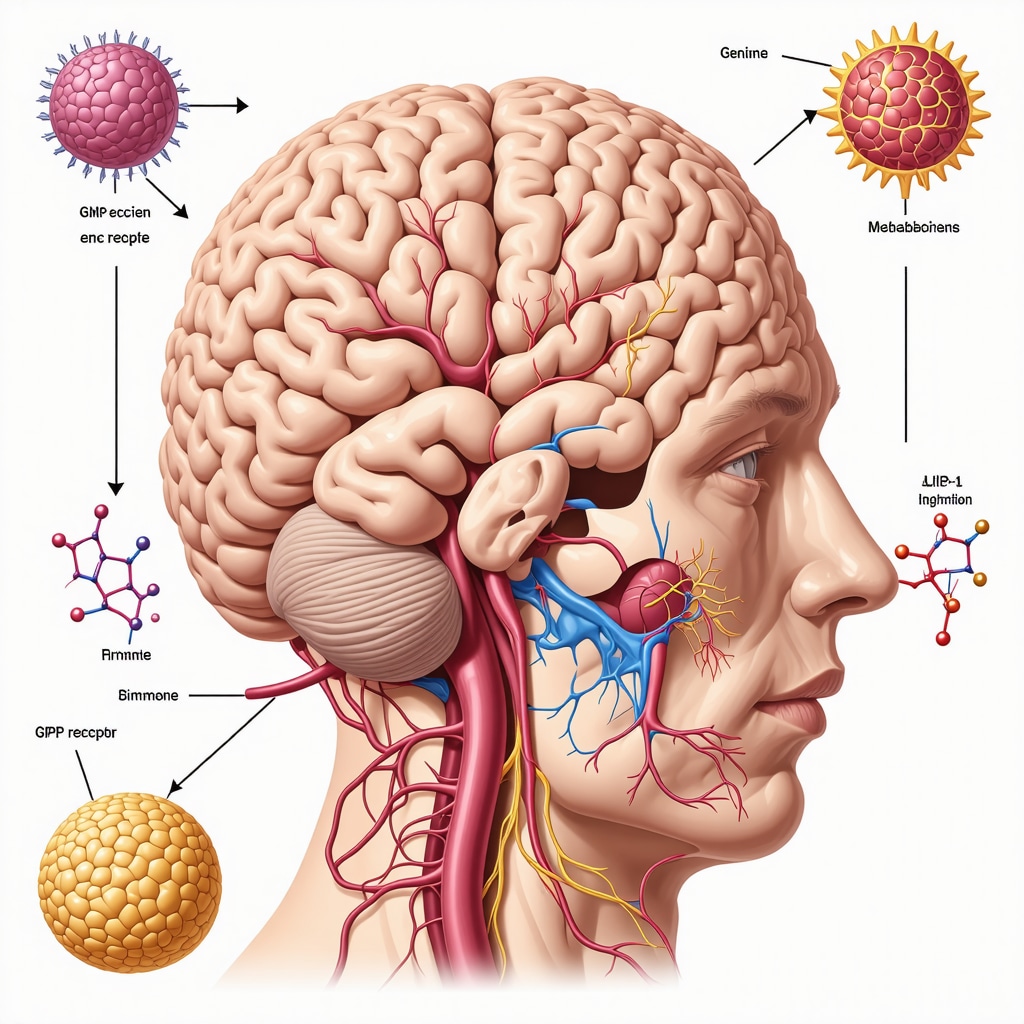
Prescription weight loss pills are not mere appetite suppressants; many function through sophisticated pathways such as glucagon-like peptide-1 (GLP-1) receptor agonism, which regulates hunger, insulin secretion, and satiety signals. For example, drugs like semaglutide and tirzepatide have revolutionized obesity management by mimicking natural hormones that promote fullness and enhance metabolic control. This nuanced pharmacology offers patients a powerful, clinically validated tool to achieve significant fat loss while reducing cardiovascular and metabolic risks.
How Do These Prescription Pills Compare to Traditional Weight Loss Methods?
Unlike standard caloric restriction or exercise alone, GLP-1 receptor agonists and other FDA-approved medications provide biochemical support that addresses underlying physiological drivers of obesity. Clinical trials demonstrate that patients using these medications can lose 10-15% of their body weight on average, outperforming lifestyle modifications alone. However, the best outcomes often arise when prescription pills are integrated into comprehensive, doctor-led weight loss plans that include behavioral counseling and nutrition guidance, ensuring safety and long-term efficacy.
Tailoring Treatment: Matching Prescription Pills to Individual Needs
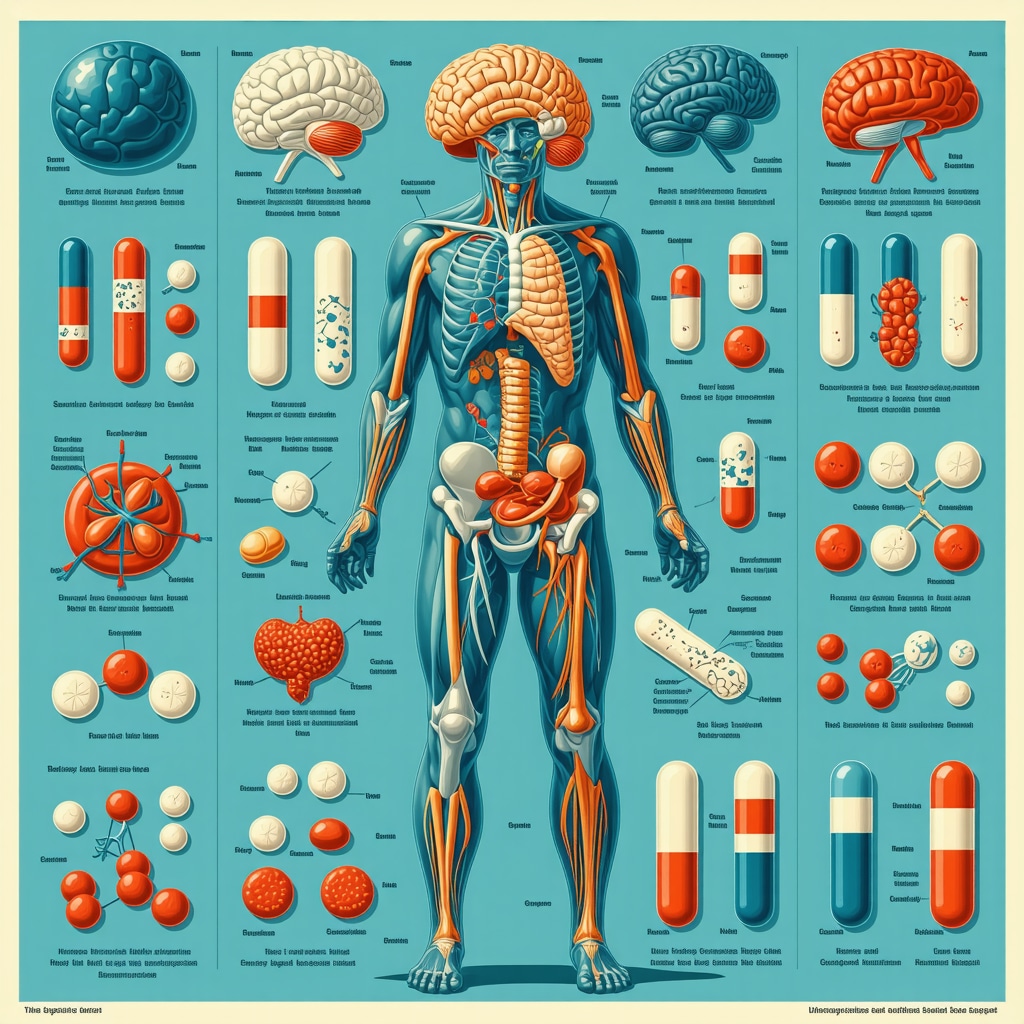
Each patient’s weight loss journey is unique, influenced by genetics, comorbidities, and lifestyle factors. Physicians carefully evaluate candidates for weight loss medications by considering medical history, potential side effects, and drug interactions. Commonly prescribed options, such as orlistat, phentermine-topiramate, and liraglutide, each offer distinct benefits and risk profiles. For instance, orlistat works by inhibiting fat absorption, whereas phentermine-topiramate suppresses appetite through central nervous system effects. Selecting the right medication involves a personalized approach that optimizes safety and effectiveness.
What Are the Safety Considerations and Side Effects to Keep in Mind?
While prescription weight loss pills provide promising results, understanding their safety profile is crucial. Side effects can range from mild gastrointestinal discomfort to rare but serious events like pancreatitis or cardiovascular concerns. Ongoing monitoring by healthcare providers ensures timely identification and management of adverse reactions. The FDA rigorously evaluates these medications, approving only those with a favorable risk-benefit ratio supported by robust clinical data, as detailed in official FDA guidelines.
Integrating Prescription Pills into a Holistic Weight Loss Strategy
Successful weight loss transcends medication alone. Combining prescription pills with lifestyle changes, mental health support, and regular medical follow-up enhances the chances of sustained fat loss and improved overall health. Telemedicine platforms now facilitate easier access to physician-prescribed weight loss plans, providing personalized care remotely to fit modern lifestyles. Explore how these integrated approaches work effectively in practice at doctor-led fat loss plans.
Curious about which prescription pills might suit your health profile best? Join the conversation by sharing your experiences or questions below, and discover personalized guidance to navigate your weight loss journey safely.
When Medication Meets Mindset: My Personal Reflections on Weight Loss Pills
Embarking on a medically guided weight loss journey, I quickly realized that prescription pills are just one piece of a much larger puzzle. For me, the psychological component—embracing patience, staying motivated despite fluctuations, and being kind to myself—was just as crucial as any drug’s biochemical effects. The medications helped curb my appetite and regulated my metabolism, but the transformation truly unfolded when I combined these benefits with mindful eating, regular physical activity, and a supportive network.
One memorable moment was when I noticed not just the pounds shedding, but an improvement in my energy levels and mood. This holistic benefit reinforced my commitment to the journey, reminding me that weight loss is more than aesthetics—it’s about reclaiming health and vitality.
Understanding the Role of Telemedicine in Making Weight Loss Medications Accessible
As someone who initially struggled to find a convenient way to access expert guidance, I found telemedicine to be a game changer. The ability to consult with healthcare providers from home eliminated many barriers such as travel time, scheduling conflicts, and even some of the stigma associated with visiting weight loss clinics. Platforms specializing in telemedicine weight loss treatment offer personalized, physician-supervised plans that include prescription medications, lifestyle coaching, and continuous follow-up—making the whole process feel more manageable and less intimidating.
How Can You Balance Expectations and Realities When Starting Prescription Weight Loss Pills?
This question resonates deeply, especially given the myriad of success stories and, conversely, the frustrations I’ve heard from others. It’s essential to understand that while these medications can significantly aid weight loss, they’re not miracle cures. The journey requires consistent effort, patience, and sometimes adjustment of the treatment plan with your doctor.
According to a comprehensive review published in The New England Journal of Medicine, combining pharmacotherapy with lifestyle modifications yields the most sustainable results. This scientific backing aligns with my own experience—prescription pills gave me a head start, but lasting change stemmed from a broader commitment to health.
Practical Tips for Maximizing the Benefits of Your Prescription Weight Loss Plan
Drawing from personal experience and expert advice, here are some strategies that helped me:
- Maintain open communication with your healthcare provider. Regular check-ins allow for timely adjustments in medication dosage or addressing side effects.
- Set realistic, incremental goals. Celebrating small victories keeps motivation high and reinforces positive habits.
- Incorporate enjoyable physical activities. Exercise doesn’t have to be a chore; find what you love to sustain consistency.
- Prioritize nutrition. Medications can suppress appetite, but quality of food intake impacts energy and overall health.
- Leverage support networks. Whether friends, family, or online communities, sharing your journey can provide encouragement and accountability.
For those curious, diving deeper into doctor-prescribed weight loss plans can offer tailored strategies that fit your unique needs and enhance your chances of success.
Have you tried prescription weight loss pills or are considering them? What challenges or victories have you encountered? Share your story or questions in the comments below—your insights might just inspire someone else on their path.
Decoding the Complex Pharmacodynamics of Next-Generation Weight Loss Medications
Prescription weight loss drugs have evolved beyond simple appetite suppressants to encompass multifaceted mechanisms that influence metabolism at cellular and systemic levels. For instance, GLP-1 receptor agonists not only regulate appetite but also slow gastric emptying and improve insulin sensitivity, creating a synergistic effect that promotes fat oxidation and reduces adipose tissue accumulation. Tirzepatide, a dual GLP-1 and GIP (glucose-dependent insulinotropic polypeptide) receptor agonist, exemplifies this advanced pharmacology by engaging multiple hormonal pathways to maximize weight reduction and glycemic control simultaneously.
Moreover, emerging research highlights how these medications modulate central nervous system reward circuits, potentially reducing hedonic eating triggers often resistant to lifestyle interventions alone. Understanding these nuanced neuroendocrine interactions is critical for clinicians aiming to tailor therapies that address both metabolic and behavioral dimensions of obesity.
What Are the Long-Term Metabolic and Cardiovascular Implications of Sustained Use of Prescription Weight Loss Pills?
One of the most pressing questions in obesity pharmacotherapy pertains to the durability and systemic impact of these treatments over extended durations. While short-term trials consistently demonstrate significant weight loss and metabolic improvements, longitudinal data are beginning to reveal additional benefits such as reduced incidence of major adverse cardiovascular events (MACE), improved lipid profiles, and decreased markers of systemic inflammation.
A landmark study published in The New England Journal of Medicine evaluating semaglutide’s cardiovascular outcomes underscored a 20% relative risk reduction in MACE among high-risk patients. This evidences that beyond weight reduction, these medications confer cardioprotective effects likely mediated by improved endothelial function, blood pressure regulation, and anti-inflammatory actions.
However, clinicians must remain vigilant about potential adverse effects such as pancreatitis, gallbladder disease, or rare but serious psychiatric symptoms, necessitating individualized risk-benefit analyses and ongoing surveillance during treatment.
Integrating Precision Medicine and Pharmacogenomics in Weight Loss Medication Selection
Personalized medicine is increasingly pivotal in optimizing weight loss pharmacotherapy. Genetic polymorphisms affecting drug metabolism, receptor sensitivity, and hormonal pathways can influence individual responses and side effect profiles. Advances in pharmacogenomic testing hold promise to predict which patients will benefit most from specific agents such as phentermine-topiramate versus GLP-1 receptor agonists, thereby reducing trial-and-error prescribing and enhancing therapeutic efficacy.
Furthermore, integrating detailed phenotyping—including metabolic rate assessments, appetite regulation patterns, and behavioral tendencies—enables a holistic approach to drug selection. This strategy aligns with emerging models that view obesity as a heterogeneous disease with diverse pathophysiological drivers rather than a uniform condition.
How Can Clinicians Effectively Monitor and Adjust Treatment Plans to Sustain Weight Loss While Minimizing Risks?
Effective management extends beyond initiation to continuous optimization. Regular monitoring of weight trajectories, metabolic parameters, and side effect profiles facilitates timely dose adjustments or medication switches. Utilizing validated tools for appetite assessment and psychological evaluation can also identify emerging challenges such as medication tolerance or mood disturbances.
Interdisciplinary collaboration among endocrinologists, nutritionists, behavioral therapists, and primary care providers is essential to maintain momentum and support patient adherence. Employing digital health technologies, including wearable devices and telehealth platforms, enhances real-time data collection and personalized feedback, making interventions more responsive and patient-centered.
Clinicians should also educate patients about the importance of gradual, sustainable weight loss and the potential need for long-term pharmacotherapy to maintain benefits, setting realistic expectations to mitigate discontinuation due to frustration or side effects.
For those interested in exploring tailored prescription weight loss strategies informed by the latest scientific advancements, consulting with specialized medical professionals can provide comprehensive, personalized guidance. Engage with expert-led resources and communities to deepen your understanding and optimize your weight management journey.
Decoding the Complex Pharmacodynamics of Next-Generation Weight Loss Medications
Prescription weight loss drugs have evolved beyond simple appetite suppressants to encompass multifaceted mechanisms that influence metabolism at cellular and systemic levels. For instance, GLP-1 receptor agonists not only regulate appetite but also slow gastric emptying and improve insulin sensitivity, creating a synergistic effect that promotes fat oxidation and reduces adipose tissue accumulation. Tirzepatide, a dual GLP-1 and GIP (glucose-dependent insulinotropic polypeptide) receptor agonist, exemplifies this advanced pharmacology by engaging multiple hormonal pathways to maximize weight reduction and glycemic control simultaneously.
Moreover, emerging research highlights how these medications modulate central nervous system reward circuits, potentially reducing hedonic eating triggers often resistant to lifestyle interventions alone. Understanding these nuanced neuroendocrine interactions is critical for clinicians aiming to tailor therapies that address both metabolic and behavioral dimensions of obesity.
What Are the Long-Term Metabolic and Cardiovascular Implications of Sustained Use of Prescription Weight Loss Pills?
One of the most pressing questions in obesity pharmacotherapy pertains to the durability and systemic impact of these treatments over extended durations. While short-term trials consistently demonstrate significant weight loss and metabolic improvements, longitudinal data are beginning to reveal additional benefits such as reduced incidence of major adverse cardiovascular events (MACE), improved lipid profiles, and decreased markers of systemic inflammation.
A landmark study published in The New England Journal of Medicine evaluating semaglutide’s cardiovascular outcomes underscored a 20% relative risk reduction in MACE among high-risk patients. This evidences that beyond weight reduction, these medications confer cardioprotective effects likely mediated by improved endothelial function, blood pressure regulation, and anti-inflammatory actions.
However, clinicians must remain vigilant about potential adverse effects such as pancreatitis, gallbladder disease, or rare but serious psychiatric symptoms, necessitating individualized risk-benefit analyses and ongoing surveillance during treatment.
Integrating Precision Medicine and Pharmacogenomics in Weight Loss Medication Selection
Personalized medicine is increasingly pivotal in optimizing weight loss pharmacotherapy. Genetic polymorphisms affecting drug metabolism, receptor sensitivity, and hormonal pathways can influence individual responses and side effect profiles. Advances in pharmacogenomic testing hold promise to predict which patients will benefit most from specific agents such as phentermine-topiramate versus GLP-1 receptor agonists, thereby reducing trial-and-error prescribing and enhancing therapeutic efficacy.
Furthermore, integrating detailed phenotyping—including metabolic rate assessments, appetite regulation patterns, and behavioral tendencies—enables a holistic approach to drug selection. This strategy aligns with emerging models that view obesity as a heterogeneous disease with diverse pathophysiological drivers rather than a uniform condition.
How Can Clinicians Effectively Monitor and Adjust Treatment Plans to Sustain Weight Loss While Minimizing Risks?
Effective management extends beyond initiation to continuous optimization. Regular monitoring of weight trajectories, metabolic parameters, and side effect profiles facilitates timely dose adjustments or medication switches. Utilizing validated tools for appetite assessment and psychological evaluation can also identify emerging challenges such as medication tolerance or mood disturbances.
Interdisciplinary collaboration among endocrinologists, nutritionists, behavioral therapists, and primary care providers is essential to maintain momentum and support patient adherence. Employing digital health technologies, including wearable devices and telehealth platforms, enhances real-time data collection and personalized feedback, making interventions more responsive and patient-centered.
Clinicians should also educate patients about the importance of gradual, sustainable weight loss and the potential need for long-term pharmacotherapy to maintain benefits, setting realistic expectations to mitigate discontinuation due to frustration or side effects.
For those interested in exploring tailored prescription weight loss strategies informed by the latest scientific advancements, consulting with specialized medical professionals can provide comprehensive, personalized guidance. Engage with expert-led resources and communities to deepen your understanding and optimize your weight management journey.
Frequently Asked Questions (FAQ)
What are the primary types of prescription weight loss pills currently available?
Prescription weight loss medications include several classes such as GLP-1 receptor agonists (e.g., semaglutide, liraglutide), dual agonists (e.g., tirzepatide), appetite suppressants (e.g., phentermine-topiramate), and fat absorption inhibitors (e.g., orlistat). Each has distinct mechanisms targeting physiological aspects of obesity like appetite regulation, metabolism enhancement, or fat digestion.
How do GLP-1 receptor agonists aid in sustainable weight loss?
GLP-1 receptor agonists mimic the incretin hormone GLP-1, enhancing satiety, slowing gastric emptying, and improving insulin sensitivity. This multifaceted action reduces hunger and caloric intake while promoting improved metabolic control, leading to significant and sustained weight loss supported by robust clinical trials.
Are prescription weight loss pills safe for long-term use?
Many FDA-approved weight loss drugs have demonstrated safety in long-term studies, but risks like gastrointestinal discomfort, pancreatitis, or rare psychiatric effects exist. Continuous medical supervision, personalized risk assessment, and periodic monitoring are essential to safely maintain therapy and manage side effects.
Can pharmacogenomics personalize weight loss medication choices?
Yes, emerging pharmacogenomic insights allow tailoring treatments based on individual genetic profiles affecting drug metabolism and receptor responsiveness. This precision medicine approach aims to optimize efficacy, reduce side effects, and minimize trial-and-error prescribing in obesity pharmacotherapy.
How important is combining medication with lifestyle changes?
Medication alone rarely suffices for long-term success. Integrating prescription pills with nutritional counseling, physical activity, behavioral therapy, and psychological support maximizes weight loss outcomes and helps maintain results by addressing both physiological and behavioral drivers of obesity.
What role does telemedicine play in accessing weight loss treatments?
Telemedicine expands access to expert-guided weight loss care by enabling remote consultations, prescription management, and ongoing monitoring. This convenience improves patient adherence, reduces barriers such as travel or stigma, and facilitates personalized, continuous support.
How do clinicians monitor and adjust treatment plans effectively?
Clinicians use regular assessments of weight, metabolic markers, side effect profiles, and psychological evaluations. They collaborate across specialties and leverage digital tools to optimize dosing, switch medications if necessary, and support patient adherence for sustained benefits.
What are the cardiovascular benefits of prescription weight loss pills?
Beyond weight reduction, certain medications like semaglutide have shown to reduce major adverse cardiovascular events (MACE) by improving endothelial function, blood pressure, lipid profiles, and inflammation, contributing to comprehensive cardiometabolic risk reduction.
Who is an ideal candidate for prescription weight loss medications?
Candidates typically have a BMI ≥30 kg/m² or ≥27 kg/m² with obesity-related comorbidities. Physicians evaluate medical history, contraindications, and patient preferences to individualize therapy ensuring safety and maximizing efficacy.
Trusted External Sources
- The New England Journal of Medicine (NEJM): Provides peer-reviewed clinical trials and meta-analyses on obesity pharmacotherapy and cardiovascular outcomes, essential for evidence-based insights.
- U.S. Food and Drug Administration (FDA): Offers comprehensive drug safety evaluations, approval status, and prescribing information critical for understanding regulatory perspectives and safety guidelines.
- American Diabetes Association (ADA): Supplies guidelines linking weight management with metabolic and glycemic control, informing integrated treatment approaches.
- Obesity Society: A leading professional organization delivering up-to-date research, treatment standards, and clinical practice recommendations in obesity medicine.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Offers authoritative resources on obesity pathophysiology, treatment modalities, and emerging research, enhancing foundational knowledge.
Conclusion: Synthesizing the Future of Prescription Weight Loss Pills
Prescription weight loss pills represent a transformative advancement in obesity management, leveraging sophisticated pharmacodynamics to address complex metabolic and behavioral factors. GLP-1 receptor agonists and newer agents like tirzepatide exemplify how precise hormonal modulation can yield significant, sustainable fat loss accompanied by cardiovascular and metabolic benefits.
However, optimal outcomes depend on personalized medicine approaches, integrating pharmacogenomics and comprehensive patient profiling to tailor therapies effectively. Continual monitoring and interdisciplinary collaboration ensure safety and long-term adherence, while telemedicine expands access to expert care.
Ultimately, prescription weight loss medications should be viewed as powerful adjuncts within a holistic strategy encompassing lifestyle changes and psychological support. Embracing this nuanced, evidence-based paradigm empowers patients and clinicians alike to transform obesity treatment from a fragmented challenge into a manageable, health-restoring journey.
Engage with this evolving field by sharing your experiences or questions, exploring expert resources, and consulting healthcare professionals to unlock personalized, effective weight management solutions.

This article’s detailed look at how prescription weight loss pills function beyond just appetite suppression really stands out to me. The role of GLP-1 receptor agonists like semaglutide in regulating hunger signals and improving metabolic control highlights how complex and promising these treatments are. It’s reassuring to know that these medications not only help with fat loss but also provide cardiovascular benefits, which is crucial given the common overlap of obesity with heart-related issues.
From what I’ve read and seen in patient forums, integrating medication with lifestyle changes seems key. The holistic approach—combining medication, nutrition, behavioral support, and exercise—appears to offer the best chance for sustainable results. I especially appreciate the emphasis on personalized treatment plans that consider genetic and lifestyle factors, as the “one-size-fits-all” model clearly falls short in obesity management.
I’m curious, though, about the psychological aspect the author touches on. How do others maintain motivation and patience during inevitable weight fluctuations on these medications? And what strategies have been most effective in balancing the expectations from medication effects with the realities of lifestyle adjustments? Sharing these experiences could be incredibly helpful for those starting their journey.