Understanding the Landscape of Legal Weight Loss Drugs in 2025
In the evolving field of obesity management, legal weight loss drugs have emerged as pivotal tools for patients and clinicians alike. This progression is driven not only by the rising prevalence of obesity but also by the nuanced understanding of pharmacological safety and efficacy profiles tailored to diverse populations. The 2025 landscape offers a spectrum of safe, doctor-approved options that reflect advanced clinical research and regulatory rigor, underscoring the importance of evidence-based weight loss strategies.
Pharmacological Innovations: The Role of GLP-1 Receptor Agonists in Safe Fat Reduction
Among the most transformative advances are GLP-1 (glucagon-like peptide-1) receptor agonists, including semaglutide and tirzepatide. These agents synergistically regulate appetite and metabolic pathways, resulting in significant fat loss with a favorable safety margin. Their mechanism of action exemplifies how targeted pharmacotherapy can harmonize with physiological processes, minimizing adverse effects while maximizing therapeutic gains. For comprehensive insights, professionals often consult expert analyses on GLP-1 medications that detail their application and patient suitability.
Ensuring Accessibility and Safety: How Telemedicine is Revolutionizing Legal Prescription Weight Loss Drugs
Telemedicine platforms have democratized access to legal weight loss prescriptions, allowing patients to engage with healthcare providers remotely. This model enhances adherence monitoring, customizes treatment plans, and facilitates timely adjustments, which are critical for safety and efficacy. The integration of telehealth aligns with modern medical paradigms emphasizing personalized, patient-centered care, as detailed in telemedicine weight loss treatment guides.
What Are the Critical Safety Considerations When Selecting Legal Weight Loss Drugs for Diverse Populations?
Safety in weight loss pharmacotherapy must be meticulously calibrated to individual health profiles, including comorbidities, age, and metabolic status. Clinicians must evaluate contraindications, potential drug interactions, and long-term effects with a lens of personalized medicine. Moreover, the psychosocial context and adherence challenges play crucial roles in therapeutic success. Authoritative guidelines from institutions like the National Institutes of Health offer evidence-based frameworks for these evaluations, emphasizing the necessity of expert oversight.
Expert-Endorsed Legal Weight Loss Drugs: A Focus on FDA-Approved Options and Their Clinical Applications
FDA-approved medications such as liraglutide, semaglutide, and orlistat exemplify the current gold standard in legal weight loss pharmacotherapy. Their clinical applications extend beyond mere weight reduction to encompass improvements in cardiovascular risk and glycemic control, reflecting their multifaceted benefits. Detailed reviews and comparative analyses can be found at the safest prescription weight loss drugs resource, which serves as a trusted compendium for healthcare professionals and patients.
Call to Action: Engage with Cutting-Edge Research and Personalized Weight Loss Strategies
For those seeking to deepen their expertise or embark on a medically guided weight loss journey, exploring customized doctor-led plans is paramount. Visit doctor-led fat loss plans to access advanced protocols designed to optimize safety and efficacy. Your insights and experiences are invaluable—consider contributing to expert forums to foster collective advancements in obesity management.
Personalized Safety Protocols: Beyond Standard Guidelines in Weight Loss Pharmacotherapy
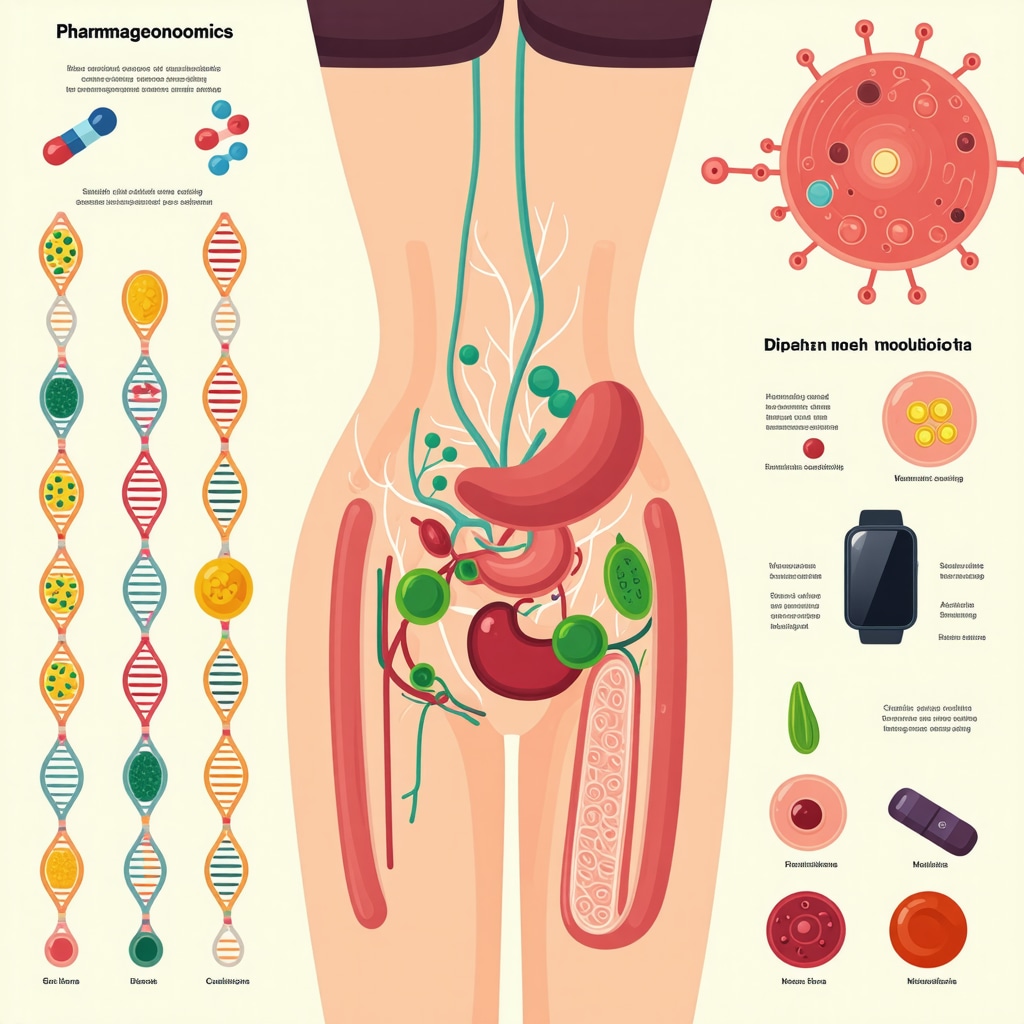
The advancement of legal weight loss drugs necessitates a move from generalized protocols to highly personalized safety assessments. This involves integrating genetic, metabolic, and lifestyle data to tailor treatment plans that minimize risks such as cardiovascular complications or gastrointestinal side effects. Clinicians are increasingly adopting pharmacogenomics to predict individual responses and optimize drug selection, dosage, and monitoring strategies.
Telemedicine’s Expanding Role: Enhancing Patient Engagement and Outcome Monitoring
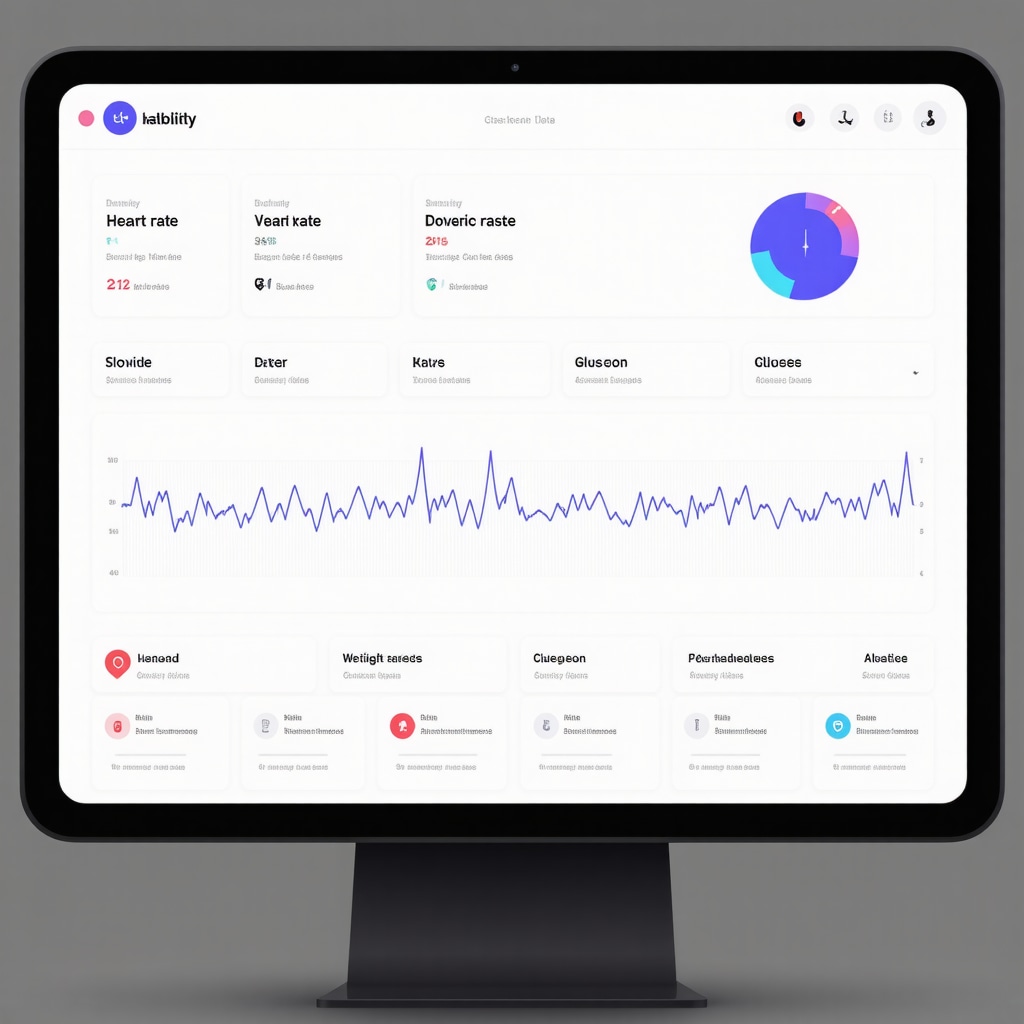
Beyond prescription access, telemedicine is evolving into a comprehensive platform for continuous patient engagement. It facilitates real-time feedback through wearable technology integration, enabling dynamic adjustments to weight loss regimens. This approach supports adherence, early detection of adverse effects, and personalized coaching, thus transforming the traditional episodic care model into a proactive, data-driven management system. Learn more about these innovations in telemedicine weight loss treatment benefits.
How Can Emerging Biomarkers and Digital Health Tools Revolutionize Safety and Effectiveness in Prescription Weight Loss Treatments?
The integration of emerging biomarkers such as gut microbiome profiles and inflammatory markers with digital health tools offers a frontier for enhancing the precision of weight loss drug therapies. These biomarkers can provide insights into individual metabolic responses and potential adverse reactions, while digital tools allow for continuous monitoring of physiological parameters and behavioral patterns. This synergy promises to refine dose titration, predict treatment outcomes, and mitigate risks, fostering a new era of personalized obesity management. A recent study published in the Journal of the American Medical Association underscores the potential impact of such integrative approaches in clinical practice.
The Intersection of Legal Weight Loss Drugs and Multi-Modal Therapeutic Strategies
Effective obesity management increasingly involves combining pharmacotherapy with behavioral, nutritional, and psychological interventions. Legal weight loss drugs serve as a critical adjunct to lifestyle modifications, enhancing satiety and metabolic efficiency to support sustainable fat reduction. Coordinated care models that include dietitians, psychologists, and exercise specialists alongside prescribing physicians ensure a holistic approach, addressing the multifactorial nature of obesity.
Leveraging FDA-Approved Drugs Within Integrated Care Frameworks for Enhanced Outcomes
Within integrated care frameworks, FDA-approved drugs like semaglutide and liraglutide are utilized not only for weight loss but also for improving comorbid conditions such as type 2 diabetes and hypertension. This dual-purpose use underscores the importance of multidisciplinary collaboration to maximize patient benefits. Clinical protocols emphasize gradual dose escalation, side effect management, and patient education to optimize adherence and long-term success. Explore detailed clinical applications at doctor-prescribed weight loss plans for sustainable results.
Call to Action: Share Your Insights on Integrating Technology and Pharmacotherapy for Safer Weight Loss
We invite healthcare professionals and patients alike to share experiences and strategies on leveraging digital health innovations in conjunction with legal weight loss drugs. Your contributions can enrich collective knowledge and drive improvements in personalized obesity treatment. Engage with our community by commenting below or exploring more on the topic through our customized doctor-led weight loss plans for sustainable success resource.
Pharmacogenomics: Tailoring Legal Weight Loss Drugs to Genetic Profiles for Optimal Safety
The burgeoning field of pharmacogenomics is revolutionizing how clinicians approach weight loss pharmacotherapy, enabling the customization of drug regimens based on individual genetic variations. Genetic polymorphisms affecting drug metabolism enzymes, such as CYP450 isoforms, can significantly alter the pharmacokinetics and pharmacodynamics of agents like semaglutide and liraglutide. By integrating genetic screening into clinical workflows, healthcare providers can anticipate adverse reactions, optimize dosing strategies, and improve therapeutic outcomes. This precision medicine approach not only enhances safety but also mitigates the risk of treatment discontinuation due to side effects.
How Does Pharmacogenomic Testing Impact Clinical Decision-Making in Weight Loss Drug Prescriptions?
Pharmacogenomic testing informs clinicians about the metabolic capacity of patients to process specific medications, providing critical insights that guide drug selection and dose titration. For example, patients with reduced function alleles in CYP2C9 may exhibit altered metabolism of certain weight loss drugs, necessitating dose adjustments or alternative therapies. Furthermore, variants in genes related to appetite regulation and energy expenditure can influence drug efficacy, allowing for more personalized treatment plans. The integration of such testing into obesity management protocols represents a paradigm shift towards individualized care, as outlined in the National Center for Biotechnology Information’s review on pharmacogenomics in obesity.
Multimodal Monitoring Frameworks: Synergizing Digital Health and Clinical Oversight for Enhanced Safety
Advanced multimodal monitoring combines wearable biosensors, mobile health applications, and electronic health records to create a comprehensive safety net around patients undergoing pharmacological weight loss treatment. Continuous glucose monitors, heart rate variability trackers, and activity sensors provide real-time physiological data, enabling clinicians to detect early signs of adverse events such as hypoglycemia or cardiovascular strain. Coupling these data streams with telehealth consultations facilitates prompt intervention and tailored regimen adjustments, fostering a responsive and patient-centric therapeutic environment.
This integrative approach addresses the complexities of polypharmacy and comorbid conditions frequently encountered in obesity management, reducing hospitalizations and improving quality of life. For a deep dive into these digital health strategies, consult the recent analysis featured in the JAMA Internal Medicine special issue on digital therapeutics.
Emerging Frontiers: Combining Legal Weight Loss Drugs with Gut Microbiota Modulators for Enhanced Metabolic Outcomes
Recent studies suggest that gut microbiota composition significantly influences obesity pathophysiology and response to pharmacotherapy. Modulating the microbiome through probiotics, prebiotics, or fecal microbiota transplantation alongside GLP-1 receptor agonists may potentiate weight loss efficacy and improve metabolic parameters. This dual approach addresses both central appetite pathways and peripheral metabolic functions, potentially minimizing drug dosages and associated side effects.
Clinical trials exploring this synergy are underway, shedding light on the potential for microbiome-informed therapeutic frameworks. Integrating microbiota assessment into patient evaluations could thus become a cornerstone of personalized obesity treatment. This frontier area is elaborated in the publication from Nature Medicine, emphasizing translational research and clinical applicability.
Integrating Behavioral Health Interventions with Pharmacotherapy: A Holistic Approach to Sustained Weight Management
Pharmacotherapy alone seldom suffices for long-term obesity control. Incorporating behavioral health strategies—such as cognitive-behavioral therapy, motivational interviewing, and stress management—addresses psychological determinants of eating behaviors and medication adherence. This multidimensional approach enhances patient engagement, mitigates relapse risk, and improves overall treatment satisfaction.
Clinicians are increasingly collaborating with mental health professionals to develop integrated care pathways that support emotional well-being alongside pharmacological interventions. This synergy is critical, as untreated psychological comorbidities often undermine pharmacotherapy effectiveness and patient safety.
What Are the Best Practices for Coordinating Behavioral and Pharmacological Treatments in Obesity Care?
Effective coordination requires interdisciplinary communication, shared decision-making frameworks, and standardized outcome metrics. Utilizing digital platforms that enable real-time data sharing among providers ensures coherent treatment plans and timely adjustments. Moreover, patient education about the interplay between behavior and pharmacotherapy fosters empowerment and adherence. Best practice guidelines from the American Psychological Association and the Obesity Society recommend embedding behavioral interventions early in the treatment continuum to maximize therapeutic synergy.
Call to Action: Advance Your Clinical Practice by Embracing Integrative, Personalized Obesity Management
Healthcare professionals are encouraged to explore and implement these cutting-edge strategies—pharmacogenomic testing, multimodal digital monitoring, microbiota modulation, and integrated behavioral health—to elevate patient safety and efficacy in weight loss treatment. Engage with our comprehensive resources and expert forums at Expert Weight Loss Management Strategies to stay abreast of emerging innovations and refine your clinical acumen.
Pharmacogenomics and Beyond: Elevating Safety Through Genomic Insights
The integration of pharmacogenomics into clinical practice marks a pivotal evolution in personalized obesity management. By discerning genetic polymorphisms that influence drug metabolism and receptor sensitivity, clinicians can tailor dosing regimens of GLP-1 receptor agonists and other FDA-approved weight loss agents with unprecedented precision. This approach mitigates adverse effects such as gastrointestinal intolerance or cardiovascular strain, enhancing both safety and adherence. Moreover, pharmacogenomic data facilitate anticipatory guidance, enabling proactive management of potential drug-drug interactions in polypharmacy contexts frequently encountered in obese populations.
Harnessing Digital Biomarkers: A New Paradigm in Continuous Therapeutic Monitoring
Emerging digital biomarkers derived from wearable biosensors and mobile health technologies advance the continuum of care by providing granular, real-time physiological and behavioral data. Metrics such as heart rate variability, glucose fluctuations, and activity patterns inform dynamic titration of weight loss medications, optimizing efficacy while preempting complications. These innovations transform traditional episodic care into a seamless, adaptive therapeutic process underpinned by data analytics and artificial intelligence-driven decision support systems.
How Do Integrative Digital Health Platforms Redefine Safety and Efficacy Monitoring in Prescription Weight Loss Treatments?
Integrative digital health platforms consolidate patient-generated health data with electronic health records, enabling a holistic view that supports precision medicine. These systems facilitate early detection of adverse events, such as hypoglycemia or excessive gastrointestinal effects, through algorithmic alerts, prompting timely clinical interventions. Additionally, patient engagement tools embedded within these platforms encourage adherence and lifestyle modifications synergistic with pharmacotherapy. A comprehensive analysis featured in JAMA Internal Medicine highlights the transformative impact of such platforms on chronic disease management, including obesity.
Synergistic Therapeutic Frontiers: Microbiome Modulation Coupled with Pharmacotherapy
Recent translational research elucidates the bidirectional interactions between gut microbiota and weight loss pharmacodynamics. Modulating microbiota composition through probiotics, prebiotics, or fecal microbiota transplantation may potentiate the efficacy of GLP-1 receptor agonists by enhancing metabolic flexibility and attenuating systemic inflammation. This integrative strategy holds promise for dose reduction and mitigation of drug-related adverse effects, thereby expanding the therapeutic window. Ongoing clinical trials are evaluating these combinations with encouraging preliminary outcomes, as detailed in Nature Medicine.
Integrated Behavioral Health: Augmenting Pharmacotherapy for Sustained Weight Management
Addressing the psychosocial dimensions of obesity is indispensable for durable treatment success. Embedding behavioral health interventions, including cognitive-behavioral therapy and motivational interviewing, within pharmacological protocols enhances patient adherence and mitigates relapse. Digital platforms fostering interdisciplinary communication and real-time data sharing underpin this integrative model, facilitating coordinated care and personalized adjustments. Professional guidelines emphasize early incorporation of behavioral strategies to maximize therapeutic synergy and patient empowerment.
Call to Action: Embrace Cutting-Edge Integration for Optimal Obesity Management
Clinicians and researchers are invited to adopt and contribute to the forefront of obesity treatment by integrating pharmacogenomic insights, digital health monitoring, microbiome modulation, and behavioral health strategies. Engage with our expert community and access advanced resources at Expert Weight Loss Management Strategies to refine clinical approaches and elevate patient outcomes through personalized, evidence-based care.
Expert Insights & Advanced Considerations
Pharmacogenomic Profiling as a Cornerstone for Personalized Weight Loss Therapy
The integration of pharmacogenomic data into prescription weight loss drug regimens marks a decisive shift towards individualized obesity management. By identifying genetic polymorphisms that influence drug metabolism and receptor sensitivity, clinicians can tailor dosing strategies of FDA-approved agents like semaglutide and liraglutide to optimize safety and efficacy, thereby reducing adverse events and enhancing adherence.
Digital Health Platforms Elevate Real-Time Safety Monitoring
Emerging integrative digital health systems consolidate continuous biomarker data from wearable biosensors with electronic health records, enabling dynamic titration of weight loss medications. This seamless monitoring facilitates early detection of side effects such as hypoglycemia or gastrointestinal intolerance, allowing timely clinical adjustments that preserve patient well-being throughout the treatment journey.
Microbiome Modulation Amplifies Pharmacotherapy Outcomes
Recent translational research underscores the synergistic potential of combining gut microbiota modulators—probiotics, prebiotics, or fecal microbiota transplantation—with GLP-1 receptor agonists. This dual approach enhances metabolic flexibility and inflammation control, potentially allowing dose reductions and minimizing drug-related adverse effects, representing an innovative frontier in obesity therapeutics.
Holistic Integration of Behavioral Health Enhances Long-Term Success
Incorporating behavioral health interventions such as cognitive-behavioral therapy and motivational interviewing alongside pharmacological treatments addresses psychological determinants of obesity. This integrative model fosters improved medication adherence, mitigates relapse risk, and supports sustained weight management, emphasizing the necessity of interdisciplinary care coordination.
Curated Expert Resources
National Institutes of Health Obesity Guidelines: Offers comprehensive, evidence-based frameworks for evaluating safety and efficacy in weight loss pharmacotherapy tailored to diverse populations, supporting clinical decision-making.
Journal of the American Medical Association (JAMA): Publishes cutting-edge research and analyses on digital therapeutics and biomarker integration in chronic disease management, including obesity, providing authoritative insights into advanced monitoring strategies.
Nature Medicine Translational Research: Features pioneering studies on gut microbiota modulation combined with pharmacotherapy, illuminating emerging synergistic treatment paradigms.
American Psychological Association & The Obesity Society Guidelines: Sets standards for embedding behavioral health interventions within obesity care, promoting interdisciplinary approaches that enhance outcomes.
LossWeight4All Expert Resources: For practical applications and detailed protocols, explore doctor-led fat loss plans and reviews of the safest prescription weight loss drugs for 2025, which serve as invaluable guides for clinicians and patients.
Final Expert Perspective
The evolving landscape of legal weight loss drugs in 2025 demands a sophisticated, personalized approach that leverages pharmacogenomics, digital health innovations, microbiome science, and integrated behavioral health. These multidimensional strategies collectively enhance safety, efficacy, and patient engagement beyond traditional paradigms. Professionals committed to excellence in obesity management should prioritize continuous learning and adoption of these advanced modalities.
We encourage healthcare providers and stakeholders to deepen their expertise by engaging with specialized resources and contributing to collaborative forums. For further guidance and to connect with expert-led initiatives, visit LossWeight4All contact page and explore tailored approaches like doctor-led fat loss plans to elevate your clinical practice and patient outcomes in this transformative era.
The article’s insight into the advancements of legal weight loss drugs in 2025 highlights a significant shift toward personalized medicine, particularly with GLP-1 receptor agonists like semaglutide. What stands out to me is the integration of telemedicine not only for prescriptions but as a platform for continuous patient engagement and real-time monitoring. In my experience, access to such digital platforms can truly make a difference in adherence and safety, especially for those balancing busy lives or living in remote areas. Additionally, the mention of pharmacogenomics shaping individualized dosing regimes is fascinating; it reflects how genomic data is becoming crucial in tailoring treatments that maximize benefits and minimize side effects. I wonder, though, as these technologies become more common, how are healthcare systems preparing for equitable access across different populations? Are there ongoing efforts to address disparities in telemedicine availability or genetic testing affordability? It would be interesting to hear from others about how they see these innovations influencing patient outcomes in diverse clinical and socio-economic environments.
Isabel raises important questions regarding equitable access to telemedicine and pharmacogenomic testing in weight loss treatments. From my perspective working in a community health setting, while telemedicine has expanded reach considerably, challenges remain—especially in rural or underserved populations lacking reliable internet or digital literacy. Some health systems are piloting programs that combine telehealth with local clinic visits or community health workers to bridge these gaps, which seems promising for improving adherence and safety monitoring.
Regarding pharmacogenomics, cost and availability still limit widespread use, but initiatives to incorporate genetic testing into standard obesity management protocols are underway in some centers. Insurance coverage and education for both providers and patients are critical to ensure these innovations don’t widen disparities.
I also appreciate the article’s emphasis on personalized safety protocols integrating genetic, metabolic, and lifestyle factors. This tailored approach aligns with what I’ve seen improve patient outcomes beyond generic treatments.
Given these advancements, I’m curious how others have navigated technology adoption challenges in diverse clinical settings. Have any readers encountered effective strategies to promote equitable access to telemedicine or pharmacogenomic-guided therapy in their practice or personal experience? Sharing such insights would be invaluable to this evolving field.”
This article provides an impressive overview of how the landscape of weight loss medications is evolving in 2025, especially with the emergence of GLP-1 receptor agonists like semaglutide and tirzepatide. From my own practice experience, I’ve seen these drugs transform patient outcomes, not just in terms of weight reduction but also with improvements in metabolic health. The integration of telemedicine platforms is especially encouraging, as it allows for more personalized oversight and real-time adjustments, which are crucial for safety and efficacy. However, I wonder about the barriers many patients face when it comes to accessing these advanced therapies—cost, insurance coverage, and health literacy being significant factors. Have others also encountered difficulties in ensuring equitable access? Additionally, the potential of pharmacogenomics to tailor treatments fascinates me—do you think this will soon become standard practice, or is it still primarily within research settings? Understanding how to implement these cutting-edge tools broadly remains a challenge but also offers exciting opportunities for truly personalized obesity care.
This post provides a very comprehensive look at how far legal weight loss drugs have come in 2025, especially with the rise of GLP-1 receptor agonists like semaglutide. From my experience working in a suburban clinic, I’ve seen patients benefit greatly from these targeted therapies, yet I’m also aware that access can still be a hurdle for many, particularly in underserved communities. Telemedicine has indeed opened doors, but challenges like digital literacy and internet connectivity still limit reach in certain areas.
Regarding pharmacogenomics, I believe wider integration could personalize treatments further, but cost remains a barrier. Do you think insurance companies and healthcare systems are making enough progress to ensure these innovative approaches are equitable? And what strategies have you found effective in overcoming these disparities in your practice? Sharing successful models could help us all improve patient outcomes across diverse populations.