Revolutionizing Fat Loss: The Rise of Injectable Weight Loss Medication
Injectable weight loss medications have emerged as a transformative option for individuals seeking effective, medically supervised fat loss solutions. Unlike traditional oral pills, these injectable therapies offer enhanced bioavailability and targeted mechanisms that can lead to significant weight reduction when combined with lifestyle changes. This new era of fat loss treatment is not just about shedding pounds; it’s about harnessing cutting-edge pharmacology to optimize metabolic health safely and sustainably.
Unlocking the Science: How Do Injectable Weight Loss Medications Work?
Medications like GLP-1 receptor agonists, including semaglutide and tirzepatide, mimic naturally occurring hormones that regulate appetite and glucose metabolism. By enhancing satiety signals and delaying gastric emptying, these injections help reduce caloric intake and improve insulin sensitivity. This dual action not only supports weight loss but also mitigates risks associated with type 2 diabetes and cardiovascular disease, making injectable treatments a multifaceted approach to obesity management. Notably, these therapies represent a paradigm shift from traditional weight loss drugs, emphasizing hormonal modulation over central nervous system stimulation.
What Are the Real-World Experiences Behind These Medications?
Consider Sarah, a 42-year-old patient who struggled with weight plateau despite rigorous diet and exercise. Under physician guidance, she began a semaglutide injection regimen. Within months, Sarah experienced a 15% reduction in body weight accompanied by improved energy levels and better glycemic control. Her journey exemplifies how injectable medications can catalyze meaningful changes when integrated with personalized medical plans. However, it’s crucial to recognize that individual responses vary, and a comprehensive evaluation by a healthcare provider is essential before starting any injectable therapy.
Injectable Weight Loss Medication: What Are the Potential Side Effects and Safety Concerns?
While these medications are generally well-tolerated, common side effects include nausea, gastrointestinal discomfort, and occasional injection site reactions. More serious but rare adverse events require vigilance, underscoring the importance of medical supervision. Additionally, contraindications such as personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 must be screened to ensure patient safety. Continuous monitoring enhances trustworthiness and optimizes therapeutic outcomes, aligning with the rigorous standards set by regulatory agencies like the FDA. For a detailed overview of safe injectable options, explore this comprehensive guide on FDA-approved weight loss injections.
How Do Injectable Weight Loss Medications Compare to Other Prescription Treatments?
Injectable therapies often outperform traditional oral weight loss drugs in efficacy and sustainability. For instance, GLP-1 agonists not only promote weight loss but also improve metabolic parameters, unlike many appetite suppressants that solely target hunger. However, accessibility, cost, and patient preference influence treatment choices. A balanced decision should consider these factors alongside clinical evidence and individual health profiles. To understand various options, including the latest innovations, visit innovative obesity drug solutions in 2024.
If you’re considering injectable weight loss medication, consult a healthcare professional who can tailor a physician-led fat loss plan to your unique needs. For expert guidance, reach out to our medical specialists here.
Injectable weight loss medications mark a pivotal advancement in obesity treatment, blending science with personalized care to unlock healthier futures.
Personalizing the Path: My Experience with Injectable Weight Loss Medications
When I first heard about injectable weight loss medications, I was both curious and cautious. The idea of an injection to aid fat loss seemed futuristic, almost too good to be true. But after months of stubborn plateaus and inconsistent results with traditional methods, I decided to explore this option under the supervision of a trusted physician. What struck me immediately was the holistic approach – it wasn’t just about the medication itself, but how it complemented lifestyle modifications tailored to my unique metabolic needs.
One of the most eye-opening aspects was how the medication influenced my appetite. I noticed a natural reduction in cravings and a sense of fullness that wasn’t forced but genuinely felt. This subtle shift in hunger cues allowed me to make better food choices without feeling deprived. Coupled with gradual improvements in my energy levels, it felt like my body was finally cooperating instead of resisting change.
Understanding the Balance: Managing Side Effects and Expectations
Of course, no treatment is without its challenges. In the initial weeks, I experienced mild nausea and some gastrointestinal discomfort, which my healthcare provider had prepared me for. Knowing these were temporary and manageable made the process less daunting. Through regular check-ins and adjustments, we ensured the treatment stayed aligned with my health goals and minimized adverse effects. This personalized monitoring is something I highly recommend for anyone considering this route.
Could Injectable Weight Loss Medications Be Right for You?
It’s natural to wonder if these medications could fit into your own health journey. Are you someone who has struggled with weight despite lifestyle efforts? Do you want a medically guided solution that respects your body’s signals rather than forcing drastic measures? These questions are crucial because injectable therapies, especially GLP-1 receptor agonists, are not one-size-fits-all but powerful tools when matched with the right support system.
Research published by the National Institutes of Health highlights the effectiveness of these medications in not only reducing weight but improving metabolic health markers over time. This scientific backing, combined with personal stories like mine, builds confidence in the treatment’s potential.
Integrating Medical Innovation with Lifestyle: The Future of Sustainable Weight Loss
What excites me most about injectable weight loss medications is how they open doors to combining medical innovation with everyday habits. These medications don’t replace the importance of diet and exercise but amplify their benefits. I found that pairing my injection regimen with mindful eating and consistent activity created a positive feedback loop, encouraging me to stay motivated and engaged.
If you’re curious about starting your own journey or want to explore physician-led fat loss plans that can be tailored just for you, check out these personalized programs. They offer insights into how medical expertise and innovative treatments work hand in hand to support long-term success.
Have you tried injectable weight loss medications or considered consulting a healthcare provider about them? I’d love to hear your experiences or questions – sharing our stories helps demystify this evolving field and builds a supportive community. Drop a comment below or reach out through this contact page. Together, we can navigate the path to healthier, sustainable weight management.
Precision Pharmacology: Tailoring Injectable Weight Loss Medications to Individual Metabolic Profiles
Injectable weight loss medications like GLP-1 receptor agonists are not a one-dimensional solution; rather, they demand a nuanced understanding of individual metabolic heterogeneity for optimal outcomes. Differences in genetic predispositions, gut microbiota composition, and hormonal milieu can influence both efficacy and tolerability. For example, polymorphisms affecting GLP-1 receptor sensitivity may modulate patient response, underscoring the importance of personalized dosing strategies and close metabolic monitoring. Integrating advanced biomarkers such as fasting insulin levels, HbA1c trajectories, and appetite-regulating peptide profiles can help clinicians refine treatment plans, balancing efficacy with side effect mitigation.
This precision approach transforms injectable therapy from a standardized regimen into a dynamic, patient-centric intervention, enhancing adherence and long-term sustainability.
What emerging biomarkers and diagnostic tools enhance the personalization of injectable weight loss therapies?
Emerging research highlights several promising biomarkers that can predict and monitor response to injectable weight loss medications. For instance, measuring levels of fibroblast growth factor 21 (FGF21), a hormone involved in energy homeostasis, can provide insight into metabolic adaptability. Additionally, continuous glucose monitoring (CGM) offers real-time data on glycemic fluctuations influenced by GLP-1 receptor agonists, facilitating dose adjustments that optimize glucose control while minimizing hypoglycemia risk. Advances in gut microbiome sequencing also open avenues to understand how microbiota-mediated metabolism impacts drug efficacy and side effects such as gastrointestinal discomfort.
These tools collectively enable a more refined therapeutic approach, moving beyond the traditional ‘‘trial and error’’ method.
Optimizing Combination Therapies: Synergistic Approaches with Injectable Weight Loss Medications
Beyond monotherapy, combining injectable weight loss drugs with adjunctive treatments is gaining traction to potentiate fat loss and metabolic benefits. For example, pairing GLP-1 receptor agonists with sodium-glucose cotransporter-2 (SGLT2) inhibitors can simultaneously enhance glycemic control and promote caloric loss through urinary glucose excretion. Moreover, emerging dual- and tri-agonists that target multiple incretin pathways, such as GLP-1, GIP, and glucagon receptors, represent the frontier of pharmacological innovation, offering superior weight reduction and metabolic improvements.
Integrating these medications with structured lifestyle interventions—tailored nutrition plans emphasizing macronutrient balance and resistance training protocols to preserve lean mass—maximizes therapeutic synergy. This multimodal strategy addresses not only adiposity but also the underlying metabolic dysfunctions that perpetuate obesity.
Long-Term Safety Profiles and Monitoring: Navigating Complexities in Chronic Use
While injectable weight loss medications have demonstrated robust short-term efficacy, their long-term safety profiles require vigilant assessment. Chronic modulation of incretin pathways may impact pancreatic function, gallbladder health, and cardiovascular systems. Regular imaging and biochemical panels to monitor pancreatic enzymes, gallbladder status, and cardiovascular markers are recommended in prolonged therapy scenarios. Additionally, understanding the risk-benefit balance in populations with pre-existing conditions, such as chronic kidney disease or thyroid disorders, is critical to prevent adverse outcomes.
Ongoing post-marketing surveillance and registries contribute invaluable real-world data, informing guideline refinements and patient counseling.
For a comprehensive review on safety monitoring protocols, see the New England Journal of Medicine’s 2019 review on incretin-based therapies.

Advanced Injection Techniques: Minimizing Discomfort and Enhancing Patient Compliance
Optimizing the administration technique of injectable weight loss medications is pivotal for patient adherence and comfort. Techniques such as rotating injection sites within the abdominal area or thigh, using fine-gauge needles, and employing prefilled auto-injectors reduce injection site reactions. Training patients on proper skin preparation and injection angle can further mitigate localized irritation. Additionally, emerging technologies like microneedle patches and sustained-release formulations promise less invasive delivery, potentially revolutionizing patient experience and expanding accessibility.
Understanding these nuances empowers patients and providers alike to maintain consistent therapy engagement, critical for achieving sustained weight loss.
If you’re seeking to deepen your understanding of injectable weight loss therapies or explore personalized treatment strategies, don’t hesitate to consult with specialized healthcare professionals who can provide tailored guidance based on the latest clinical evidence.
Precision Pharmacology: Tailoring Injectable Weight Loss Medications to Individual Metabolic Profiles
Injectable weight loss medications like GLP-1 receptor agonists are not a one-dimensional solution; rather, they demand a nuanced understanding of individual metabolic heterogeneity for optimal outcomes. Differences in genetic predispositions, gut microbiota composition, and hormonal milieu can influence both efficacy and tolerability. For example, polymorphisms affecting GLP-1 receptor sensitivity may modulate patient response, underscoring the importance of personalized dosing strategies and close metabolic monitoring. Integrating advanced biomarkers such as fasting insulin levels, HbA1c trajectories, and appetite-regulating peptide profiles can help clinicians refine treatment plans, balancing efficacy with side effect mitigation.
This precision approach transforms injectable therapy from a standardized regimen into a dynamic, patient-centric intervention, enhancing adherence and long-term sustainability.
What emerging biomarkers and diagnostic tools enhance the personalization of injectable weight loss therapies?
Emerging research highlights several promising biomarkers that can predict and monitor response to injectable weight loss medications. For instance, measuring levels of fibroblast growth factor 21 (FGF21), a hormone involved in energy homeostasis, can provide insight into metabolic adaptability. Additionally, continuous glucose monitoring (CGM) offers real-time data on glycemic fluctuations influenced by GLP-1 receptor agonists, facilitating dose adjustments that optimize glucose control while minimizing hypoglycemia risk. Advances in gut microbiome sequencing also open avenues to understand how microbiota-mediated metabolism impacts drug efficacy and side effects such as gastrointestinal discomfort.
These tools collectively enable a more refined therapeutic approach, moving beyond the traditional ‘‘trial and error’’ method.
Optimizing Combination Therapies: Synergistic Approaches with Injectable Weight Loss Medications
Beyond monotherapy, combining injectable weight loss drugs with adjunctive treatments is gaining traction to potentiate fat loss and metabolic benefits. For example, pairing GLP-1 receptor agonists with sodium-glucose cotransporter-2 (SGLT2) inhibitors can simultaneously enhance glycemic control and promote caloric loss through urinary glucose excretion. Moreover, emerging dual- and tri-agonists that target multiple incretin pathways, such as GLP-1, GIP, and glucagon receptors, represent the frontier of pharmacological innovation, offering superior weight reduction and metabolic improvements.
Integrating these medications with structured lifestyle interventions—tailored nutrition plans emphasizing macronutrient balance and resistance training protocols to preserve lean mass—maximizes therapeutic synergy. This multimodal strategy addresses not only adiposity but also the underlying metabolic dysfunctions that perpetuate obesity.
Long-Term Safety Profiles and Monitoring: Navigating Complexities in Chronic Use
While injectable weight loss medications have demonstrated robust short-term efficacy, their long-term safety profiles require vigilant assessment. Chronic modulation of incretin pathways may impact pancreatic function, gallbladder health, and cardiovascular systems. Regular imaging and biochemical panels to monitor pancreatic enzymes, gallbladder status, and cardiovascular markers are recommended in prolonged therapy scenarios. Additionally, understanding the risk-benefit balance in populations with pre-existing conditions, such as chronic kidney disease or thyroid disorders, is critical to prevent adverse outcomes.
Ongoing post-marketing surveillance and registries contribute invaluable real-world data, informing guideline refinements and patient counseling.
For a comprehensive review on safety monitoring protocols, see the New England Journal of Medicine’s 2019 review on incretin-based therapies.
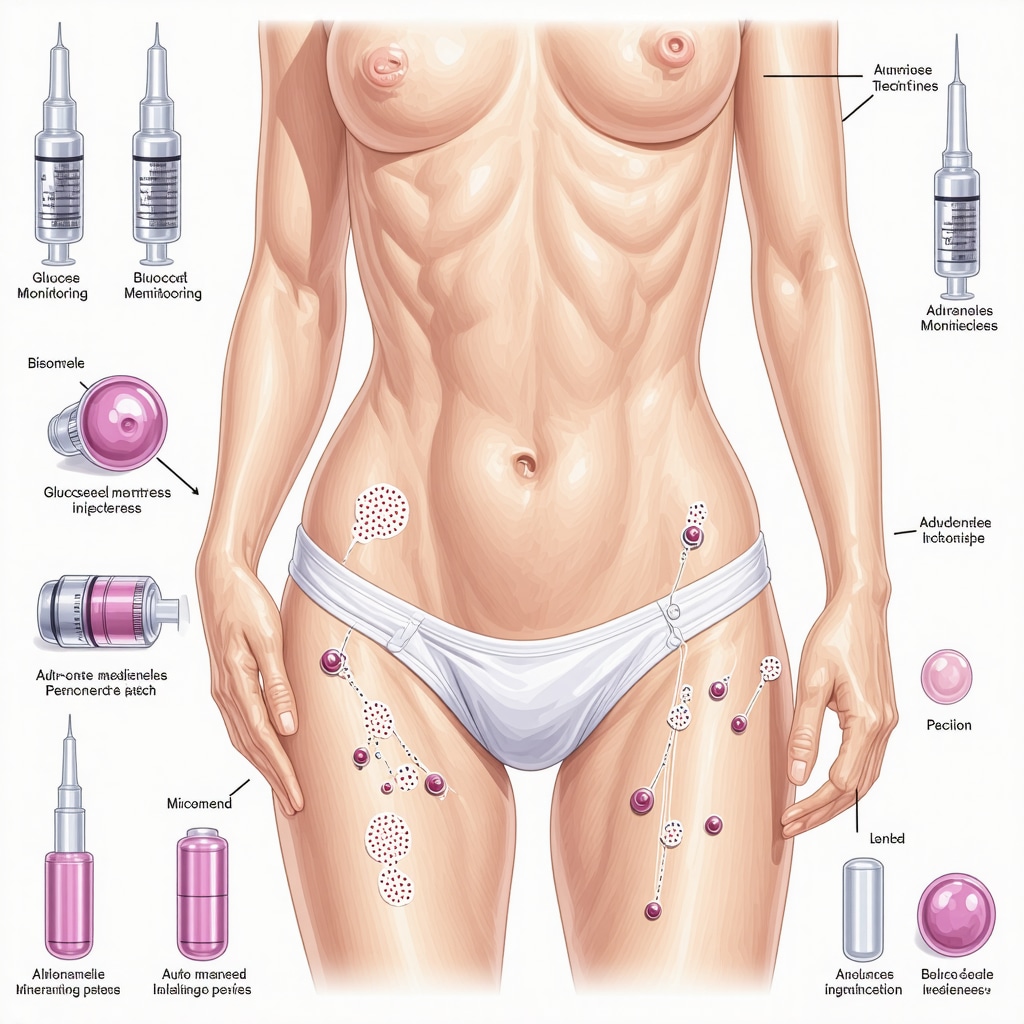
Advanced Injection Techniques: Minimizing Discomfort and Enhancing Patient Compliance
Optimizing the administration technique of injectable weight loss medications is pivotal for patient adherence and comfort. Techniques such as rotating injection sites within the abdominal area or thigh, using fine-gauge needles, and employing prefilled auto-injectors reduce injection site reactions. Training patients on proper skin preparation and injection angle can further mitigate localized irritation. Additionally, emerging technologies like microneedle patches and sustained-release formulations promise less invasive delivery, potentially revolutionizing patient experience and expanding accessibility.
Understanding these nuances empowers patients and providers alike to maintain consistent therapy engagement, critical for achieving sustained weight loss.
If you’re seeking to deepen your understanding of injectable weight loss therapies or explore personalized treatment strategies, don’t hesitate to consult with specialized healthcare professionals who can provide tailored guidance based on the latest clinical evidence.
Frequently Asked Questions (FAQ)
What are injectable weight loss medications, and how do they differ from oral weight loss drugs?
Injectable weight loss medications, primarily GLP-1 receptor agonists like semaglutide and tirzepatide, are administered via subcutaneous injections and act hormonally to reduce appetite and improve metabolism. Unlike oral drugs that often rely on central nervous system stimulation or appetite suppression, injectables mimic natural hormones, offering enhanced bioavailability, targeted action, and typically greater efficacy in sustained fat loss.
Who is an ideal candidate for injectable weight loss therapy?
Ideal candidates include adults with obesity (BMI >30) or overweight individuals (BMI >27) with comorbidities such as type 2 diabetes or cardiovascular risk factors. It is essential that patients undergo a comprehensive medical evaluation to exclude contraindications (e.g., personal or family history of medullary thyroid carcinoma) and to ensure commitment to lifestyle modifications alongside medication.
What side effects should patients expect, and how can they be managed?
Common side effects include nausea, gastrointestinal discomfort, and injection site reactions. These are usually transient and manageable with dose titration, hydration, and dietary adjustments. Serious adverse events are rare but require prompt medical attention. Continuous monitoring by healthcare providers helps mitigate risks and tailor treatment plans accordingly.
Can injectable weight loss medications be combined with other treatments?
Yes, combination therapies are increasingly utilized to maximize benefits. For example, GLP-1 receptor agonists may be paired with SGLT2 inhibitors or emerging dual-/tri-agonists targeting multiple metabolic pathways. Combining pharmacotherapy with structured nutrition and exercise regimens further enhances fat loss and metabolic health.
How personalized is injectable weight loss treatment?
Personalization is integral, considering genetic factors, gut microbiome profiles, hormonal milieu, and emerging biomarkers such as FGF21 and continuous glucose monitoring data. This precision pharmacology approach refines dosing and optimizes efficacy while minimizing side effects, moving beyond ‘‘trial and error’’ to patient-centric care.
What are the long-term safety considerations?
Long-term use requires vigilant monitoring of pancreatic, gallbladder, and cardiovascular health. Regular imaging and laboratory assessments are recommended. Post-marketing surveillance continues to inform safety profiles, especially in patients with pre-existing conditions. Collaborative decision-making ensures risk-benefit balance is maintained.
How do advanced injection techniques improve patient experience?
Techniques like rotating injection sites, using fine-gauge needles, and prefilled auto-injectors reduce discomfort and local reactions. Emerging delivery methods like microneedle patches and sustained-release formulations offer promising, less invasive alternatives, which may increase adherence and accessibility.
Are injectable weight loss medications suitable for everyone struggling with obesity?
While highly effective for many, these medications are not universally appropriate. Patients with certain medical histories or contraindications must avoid them. Additionally, they should be viewed as adjuncts to—not replacements for—comprehensive lifestyle modifications and medical supervision.
How soon can patients expect to see results?
Weight loss onset varies, but many patients observe meaningful reductions within weeks to months. Continuous adherence, dose adjustments, and lifestyle integration influence outcomes. Early improvements in appetite and glycemic control often precede significant fat loss.
Where can patients find physician-led injectable weight loss plans?
Specialized clinics and medically supervised programs offer tailored injectable therapy combined with nutrition and exercise counseling. Resources such as physician-led fat loss plans can guide patients to expert care aligned with their unique metabolic needs.
Trusted External Sources
- National Institutes of Health (NIH) – Obesity and Metabolic Research: Provides peer-reviewed clinical studies and meta-analyses on injectable medications’ efficacy and safety, underpinning evidence-based practice.
- U.S. Food and Drug Administration (FDA): Offers authoritative approvals, labeling information, and safety communications for weight loss injectables, ensuring regulatory compliance and patient safety.
- New England Journal of Medicine (NEJM) – Review on Incretin-Based Therapies: Presents comprehensive evaluations of long-term safety profiles and mechanistic insights into GLP-1 receptor agonists and related agents.
- American Diabetes Association (ADA): Publishes guidelines integrating injectable weight loss medications within diabetes and obesity management, highlighting clinical best practices.
- Obesity Society: A leading professional organization providing clinical guidelines, emerging research updates, and educational materials on pharmacological obesity treatments.
Conclusion: Expert Takeaway on Injectable Weight Loss Medications
Injectable weight loss medications represent a landmark advancement in obesity treatment, offering targeted hormonal modulation that transcends traditional appetite suppression. Their efficacy in promoting sustained fat loss, improving metabolic health, and reducing comorbid risks signifies a paradigm shift toward precision pharmacology tailored to individual metabolic profiles. While side effects and long-term safety necessitate vigilant monitoring, the synergy of these medications with personalized lifestyle interventions amplifies therapeutic success. As innovative delivery techniques and combination therapies continue to evolve, injectable treatments are poised to become integral components of comprehensive obesity management.
For anyone seeking medically guided, effective fat loss strategies, consulting specialized healthcare providers to explore physician-led injectable programs is a prudent step. Share your experiences, ask questions, and engage with expert content to empower your journey toward healthier, sustainable weight management.

I’ve been reading about injectable weight loss medications like semaglutide and tirzepatide, and this post really clarifies how they work differently from traditional oral pills. The focus on hormonal modulation rather than just appetite suppression or CNS stimulation seems like a promising shift for effective and sustainable weight loss. What intrigues me most is how these injections don’t just reduce appetite but also improve insulin sensitivity, addressing metabolic health comprehensively. However, I wonder about the variability in individual responses. Given that genetics and gut microbiota play a role in how patients respond to these treatments, how accessible is personalized metabolic profiling in typical clinical settings? It seems essential for maximizing benefits and minimizing side effects, but I’m curious if the average patient could realistically expect this level of customization, or is it mostly available at specialized centers? Additionally, considering the initial side effects like nausea and gastrointestinal discomfort, how have others managed these effectively without feeling discouraged early on? I’d love to hear experiences or tips from those who have navigated the early stages of injectable therapy. Has anyone noticed the balance between medication and lifestyle adjustments truly impacting long-term success? It feels like combining cutting-edge science with personalized care could redefine obesity management, but practical insights would really help demystify the journey for newcomers.
This post provides a comprehensive look at how injectable weight loss medications are shaping the future of obesity management. I’ve personally seen a few friends succeed with medications like semaglutide, especially when combined with a solid lifestyle plan. What stands out is the emphasis on customizing treatment based on individual metabolic profiles—something that seems to elevate weight management from a one-size-fits-all approach to truly personalized care. That said, I wonder how long it will take for routine clinics to incorporate advanced biomarkers and genetic profiling into their standard diagnostic processes. Are we still mostly in the realm of specialized centers? Also, I found the section on managing side effects really practical; many early nausea symptoms can be mitigated with dose adjustments and dietary tweaks, which is reassuring. For those who’ve been on these medications longer, how has your experience with long-term safety been? Do you feel confident in the ongoing monitoring protocols? I believe these innovations could make a significant difference, but widespread access and education are essential to truly transform treatment outcomes.
This article confirms how revolutionary injectable weight loss medications are becoming in addressing obesity, especially with their hormone-based approach that targets appetite and metabolism. Having followed patients on GLP-1 receptor agonists like semaglutide, I can attest to the positive impact they’ve had when combined with personalized lifestyle interventions. What I find particularly promising is the move toward precision medicine—tailoring doses and monitoring using advanced biomarkers to improve outcomes and minimize side effects.