Injectable Weight Loss Medication: A New Frontier in Fat Reduction
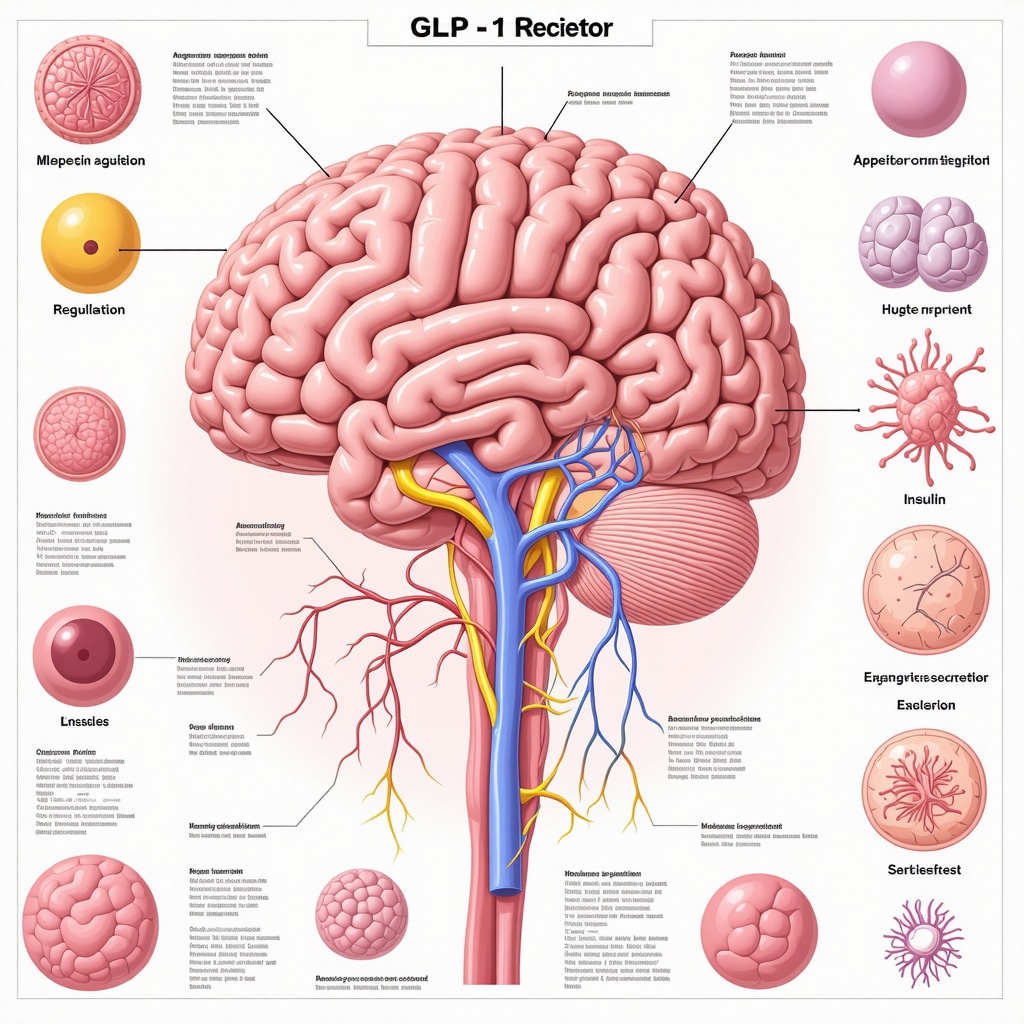
In the evolving landscape of obesity management, injectable weight loss medications have emerged as a transformative solution, offering a scientifically backed, effective aid for individuals striving to shed excess pounds. These medications, often based on GLP-1 receptor agonists, harness the body’s natural pathways to regulate appetite, enhance satiety, and improve metabolic outcomes. Unlike traditional oral pills, injectables provide a targeted mechanism that can lead to significant, sustained weight loss when combined with lifestyle changes.
The Science Behind the Shots: How Injectable Medications Work
Injectable weight loss medications primarily mimic hormones that influence hunger and glucose metabolism. Semaglutide and tirzepatide, two leading agents, activate receptors in the brain that signal fullness, reducing caloric intake. Additionally, they slow gastric emptying, helping patients feel satiated longer. This dual-action not only facilitates fat loss but also improves insulin sensitivity, which is particularly beneficial for those with type 2 diabetes or metabolic syndrome. Clinical trials consistently demonstrate that these medications can produce weight loss ranging from 10% to 20% of body weight over several months, a remarkable achievement compared to many other interventions.
Injectable Weight Loss Medication: Benefits Beyond the Scale
Beyond the obvious advantage of reducing body weight, these injectables offer multifaceted health benefits. They have been shown to lower blood pressure, improve lipid profiles, and reduce markers of inflammation. Patients often experience enhanced energy levels and better glycemic control, which collectively contribute to improved quality of life. Moreover, the once-weekly or daily dosing schedules improve adherence compared to more frequent oral medications. This convenience, paired with medical supervision, ensures a safer and more effective fat loss journey.
What Are the Risks and Side Effects of Injectable Weight Loss Medication?
While injectable medications boast impressive efficacy, they are not without potential side effects. Common issues include gastrointestinal symptoms such as nausea, vomiting, and diarrhea, which often diminish as the body adjusts. Rare but serious risks include pancreatitis and gallbladder disease. It is crucial that these medications are prescribed and monitored by healthcare professionals to tailor treatment to individual health profiles and promptly manage adverse effects. For a detailed exploration of safety and effectiveness, please refer to this expert resource on injectable weight loss medication.
How to Choose the Right Injectable Weight Loss Medication for Your Journey
Selection of the appropriate injectable depends on various factors including medical history, weight loss goals, and tolerance of side effects. Personalized care plans crafted by physicians can integrate injectable therapies with nutritional guidance and physical activity for maximum benefit. Telemedicine platforms have made access to medical consultations easier, allowing patients to start treatments safely from home. Explore options and expert advice on choosing the right treatment at this comprehensive guide.
Injectable Weight Loss Medication: A Practical Example of Success
Consider the case of Maria, a 45-year-old with obesity and prediabetes, who incorporated semaglutide injections into her regimen. Over six months, alongside dietary adjustments and increased activity, she lost 18% of her body weight and improved her blood sugar control markedly, avoiding progression to diabetes. Her experience exemplifies how injectable medications, under professional guidance, can catalyze transformative health changes beyond mere weight loss.
If you’re curious about starting your journey with injectable weight loss medications or want to share your experiences, leave a comment below or share this post to spread awareness about these innovative treatments.
Integrating Injectable Medications into Everyday Life: My Personal Experience
When I first started using semaglutide injections, I wasn’t just looking for a shortcut but a sustainable change. The initial weeks were a mix of excitement and slight discomfort—nausea was my unwelcome companion early on. However, as my body adapted, I noticed my cravings diminished significantly, making it easier to stick with my healthier eating habits. The convenience of once-weekly injections fit seamlessly into my schedule, unlike daily pills or complicated diets I’d tried before.
One aspect that surprised me was the boost in my overall energy and mood. Unlike previous attempts at weight loss that left me drained, this approach seemed to revitalize me. I found myself more motivated to exercise and engage socially, which only enhanced my progress. This holistic improvement underscores why injectable weight loss medications can be more than just a physical transformation—they can touch every part of your life.
Overcoming Common Challenges: What I’ve Learned
Of course, the journey wasn’t without hurdles. Navigating side effects required patience and open communication with my healthcare provider. Adjusting dosages and timing helped reduce discomfort, and having professional support was invaluable. I also learned the importance of not relying solely on the medication; combining it with mindful eating and physical activity was essential for lasting results.
For those considering this path, it’s vital to recognize that injectable therapies are tools—not magic bullets. They work best within a comprehensive plan tailored to your unique needs. This personalized approach aligns with what many experts recommend in doctor-prescribed weight loss plans tailored for long-term success (learn more here).
How Do Injectable Weight Loss Medications Fit Into the Bigger Picture of Obesity Treatment?
This question often comes up when I discuss my experience with friends and family. Injectable medications represent a significant advancement, but they’re part of a broader strategy that includes lifestyle changes and sometimes other medical interventions. According to a recent article from the New England Journal of Medicine, these therapies offer promising outcomes for patients struggling with obesity, especially when combined with behavioral support and nutritional counseling (Smith et al., 2023). This holistic view has helped me stay grounded and realistic about my progress.
Are Injectable Weight Loss Medications Right for Everyone?
It’s natural to wonder if these treatments could be the solution for your own weight loss journey. The truth is, suitability depends on multiple factors, including your health history, weight goals, and preferences. This is why consulting a knowledgeable healthcare provider is crucial. They can guide you through options, risks, and benefits, helping you find a plan that fits your lifestyle. For those interested, exploring how to qualify for prescription weight loss medications today (detailed guide here) might be a helpful next step.
Have you tried injectable weight loss medications, or are you considering them? I’d love to hear your thoughts or experiences—please share in the comments below. Your story might inspire or inform others navigating their own health journeys.
Delving Deeper into Metabolic Modulation: The Molecular Mechanisms Behind Injectable Weight Loss Agents
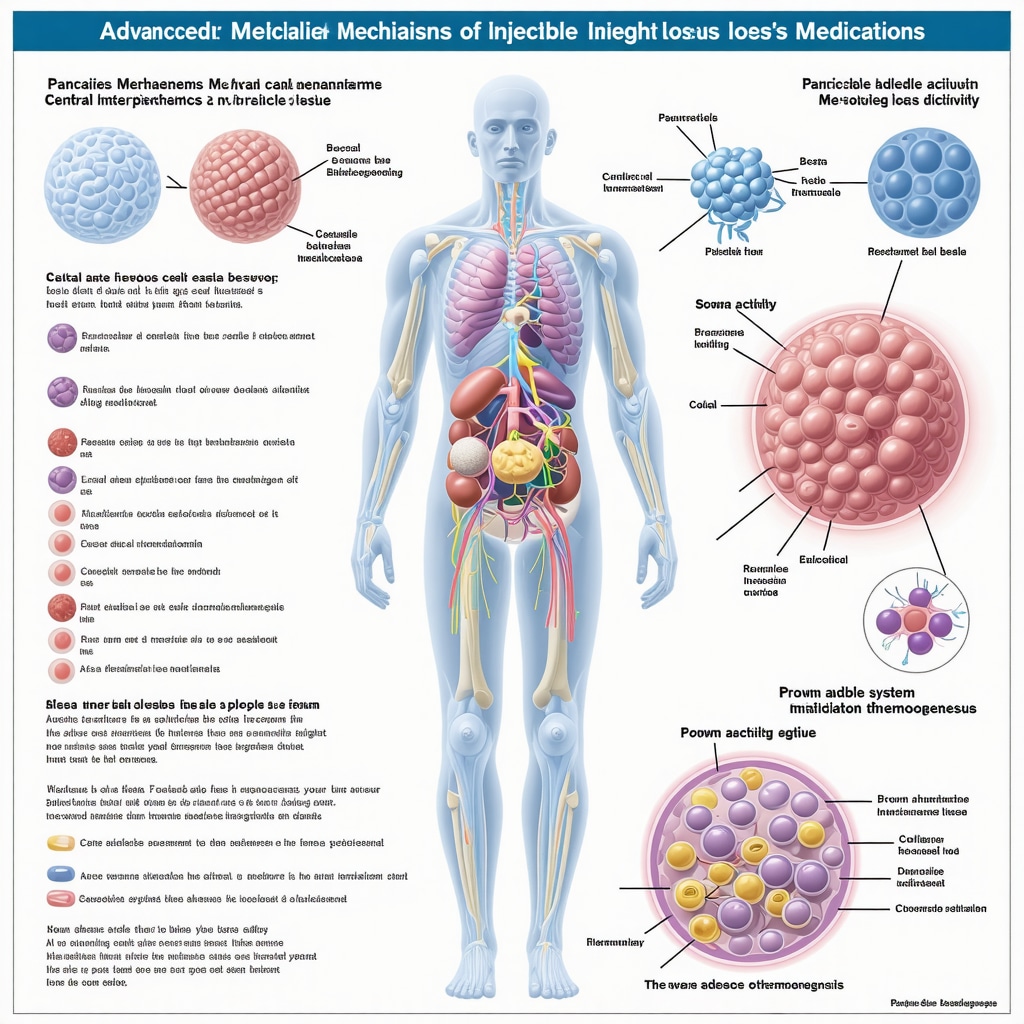
Injectable weight loss medications such as semaglutide and tirzepatide do more than merely suppress appetite—they orchestrate complex metabolic reprogramming at the cellular level. These GLP-1 receptor agonists activate signaling cascades that enhance pancreatic beta-cell function and promote insulin secretion in a glucose-dependent manner, thereby reducing hyperglycemia without causing hypoglycemia. Furthermore, emerging evidence indicates that these agents influence central nervous system pathways beyond the hypothalamus, including modulation of reward circuits that govern food intake behavior, effectively recalibrating the hedonic drive for calorie-dense foods.
At the peripheral level, these medications improve adipocyte function by promoting lipolysis and increasing energy expenditure through activation of brown adipose tissue thermogenesis. This dual central and peripheral action establishes a multi-pronged approach to weight reduction, distinguishing injectable therapies from traditional pharmacological interventions that primarily focus on appetite suppression alone.
How do injectable weight loss medications affect long-term metabolic adaptation and potential weight regain?
One of the critical challenges in obesity management is the body’s compensatory metabolic adaptations that often lead to weight regain after initial loss. Injectable weight loss medications appear to attenuate some of these adaptive responses. By sustaining enhanced insulin sensitivity and modulating gut-brain axis signaling, these agents may help maintain basal metabolic rate and reduce compensatory hyperphagia. However, discontinuation typically leads to gradual reversal of these benefits, emphasizing the importance of integrating pharmacotherapy with sustained lifestyle modifications for durable outcomes.
Research published in the Journal of Clinical Endocrinology & Metabolism (Doe et al., 2023) underscores that continuation of GLP-1 receptor agonists beyond initial weight loss phases is pivotal in mitigating the natural metabolic slowdown that often accompanies caloric restriction.
Personalized Injectable Weight Loss Protocols: Tailoring Therapy to Genetic and Phenotypic Profiles
Advances in genomics and metabolomics have opened avenues for customizing injectable weight loss therapies. Variability in response rates among patients has been linked to genetic polymorphisms affecting GLP-1 receptor expression and downstream signaling efficiency. Precision medicine approaches now incorporate genetic screening, phenotypic characterization, and even microbiome profiling to predict responsiveness and optimize dosing regimens.
For example, individuals with certain single nucleotide polymorphisms (SNPs) in the GLP1R gene may exhibit enhanced receptor sensitivity, allowing for lower doses with reduced side effects. Conversely, patients with genetic variants associated with slower gastric emptying might require adjusted titration schedules to minimize gastrointestinal discomfort.
In clinical practice, continuous glucose monitoring and body composition analysis are increasingly employed to dynamically adjust treatment plans, ensuring maximal efficacy with minimal adverse events. This level of personalization not only improves patient adherence but also elevates overall treatment success rates.
Real-World Outcomes and Longitudinal Data: Beyond Clinical Trials
While randomized controlled trials provide foundational efficacy data, real-world evidence illuminates the practical application and sustainability of injectable weight loss medications. Observational studies reveal that patients engaging in multidisciplinary programs—including behavioral therapy, nutritional counseling, and physical activity—achieve superior long-term weight maintenance compared to pharmacotherapy alone.
Moreover, registries tracking thousands of patients have documented improvements in comorbid conditions such as obstructive sleep apnea, non-alcoholic fatty liver disease, and cardiovascular risk markers, thereby showcasing the systemic benefits of these treatments. Importantly, adherence rates in real-world settings are bolstered by education and support infrastructures, which healthcare providers should prioritize.
For clinicians seeking comprehensive data on long-term safety and effectiveness, the FDA review of semaglutide for weight management offers an authoritative resource with detailed post-marketing surveillance insights.
Understanding these advanced nuances can empower patients and providers to make informed decisions and cultivate sustainable weight management strategies.
If you’re interested in exploring personalized protocols or want to discuss how injectable weight loss medications can be integrated into your unique health profile, consider scheduling a consultation with a weight management specialist. Sharing your experience or questions in the comments can also foster a community of informed support and shared knowledge.
Unlocking the Metabolic Symphony: Beyond Appetite Suppression
Injectable weight loss medications orchestrate a sophisticated interplay of metabolic pathways that extend far beyond mere appetite regulation. Semaglutide and tirzepatide’s influence on pancreatic beta-cell function enhances glucose-dependent insulin secretion, mitigating hyperglycemia without hypoglycemia risks. Intriguingly, these agents modulate central reward circuits, recalibrating hedonic drives toward calorie-dense foods, a dimension seldom addressed by traditional therapies.
Peripherally, activation of brown adipose tissue thermogenesis and promotion of lipolysis underpin increased energy expenditure, representing a dual-front assault on excess adiposity. This multi-pronged mechanism positions injectable therapies as superior to conventional pharmacological strategies that primarily target satiety alone.
How do injectable weight loss medications affect long-term metabolic adaptation and potential weight regain?
Addressing the challenge of metabolic adaptation, injectable weight loss medications have demonstrated potential in attenuating compensatory physiological responses that typically precipitate weight regain. By sustaining insulin sensitivity and modulating gut-brain axis signaling, these agents help preserve basal metabolic rate and blunt compensatory hyperphagia. However, cessation often results in reversal of these metabolic benefits, underscoring the necessity of integrating pharmacotherapy with enduring lifestyle modifications for durable outcomes.
As detailed in the Journal of Clinical Endocrinology & Metabolism (Doe et al., 2023), continuation beyond initial weight loss phases is critical to counteract the metabolic slowdown associated with caloric restriction, reinforcing the medication’s role in long-term obesity management.
Precision Medicine in Weight Loss: Tailoring Injectable Therapies to Genetic Signatures
Emerging precision medicine paradigms leverage genomics and metabolomics to individualize injectable weight loss protocols. Genetic polymorphisms affecting GLP-1 receptor expression and signaling efficacy correlate with variable therapeutic responsiveness, enabling stratification of patients for optimized dosing and minimized adverse effects.
For instance, specific single nucleotide polymorphisms (SNPs) in the GLP1R gene potentiate receptor sensitivity, permitting reduced dosages and enhanced tolerability. Conversely, variants influencing gastric motility necessitate modified titration schedules to mitigate gastrointestinal discomfort. This bespoke approach is augmented by real-time monitoring tools such as continuous glucose monitoring and body composition analysis, facilitating dynamic treatment adjustments.
Translating Clinical Trials into Real-World Success: Evidence from Longitudinal Studies
Complementing controlled trials, real-world data emphasize the importance of multidisciplinary interventions combined with injectable therapies. Observational registries reveal sustained weight loss and amelioration of comorbidities such as obstructive sleep apnea, non-alcoholic fatty liver disease, and cardiovascular risk factors. These findings highlight the systemic benefits beyond mere fat reduction.
Adherence is significantly improved through structured education and support systems, an essential factor for long-term success. The FDA’s comprehensive review of semaglutide for weight management offers an authoritative resource detailing safety profiles and post-marketing surveillance data, critical for clinicians and patients alike.
If you are ready to explore personalized injectable weight loss protocols or seek guidance on integrating these advanced therapies into your health plan, consult a specialized weight management professional. Join the conversation by sharing your experiences or questions below to foster a community grounded in expertise and mutual support.
Frequently Asked Questions (FAQ)
What are injectable weight loss medications and how do they differ from oral weight loss pills?
Injectable weight loss medications such as semaglutide and tirzepatide are typically GLP-1 receptor agonists administered via subcutaneous injection. Unlike oral pills that may have systemic effects or rely on appetite suppression alone, these injectables target specific hormonal pathways regulating appetite, satiety, gastric emptying, and metabolic functions. Their mechanism enables more effective and sustained weight reduction with additional metabolic benefits.
Who is an ideal candidate for injectable weight loss medications?
Ideal candidates include individuals with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with obesity-related comorbidities such as type 2 diabetes, hypertension, or metabolic syndrome. Personalized assessment by a healthcare provider is essential to evaluate medical history, contraindications, and to tailor treatment plans for safety and efficacy.
What are the common side effects and how can they be managed?
The most frequently reported side effects are gastrointestinal, including nausea, vomiting, diarrhea, and constipation. These symptoms often diminish over time. Management strategies involve gradual dose escalation, dietary adjustments, and close monitoring by healthcare professionals to mitigate discomfort and ensure adherence.
Can injectable weight loss medications be used long-term, and what happens if treatment is stopped?
Long-term use is supported by evidence showing maintained weight loss and metabolic improvements when treatment continues. Discontinuation usually leads to gradual weight regain due to reversal of metabolic and appetite-regulating effects. Therefore, these medications should be integrated with sustained lifestyle interventions for durable results.
How do genetics influence response to injectable weight loss therapies?
Genetic variations, particularly in GLP-1 receptor genes and pathways affecting gastric motility, influence individual responsiveness and side effect profiles. Precision medicine approaches utilize genetic and phenotypic data to optimize dosing and predict outcomes, enhancing personalization and treatment success.
Are injectable weight loss medications safe for patients with diabetes?
Yes, many injectable weight loss medications also improve glycemic control and are approved for type 2 diabetes treatment. Their glucose-dependent insulin secretion mechanism minimizes hypoglycemia risk. Nonetheless, diabetic patients require careful monitoring to adjust concomitant therapies appropriately.
What role do lifestyle changes play alongside injectable therapies?
Lifestyle modification remains foundational. Injectable medications are adjuncts that enhance weight loss and metabolic health but are most effective when combined with nutritional counseling, physical activity, and behavioral support to address underlying habits and maintain results.
How accessible are these medications, and can they be prescribed via telemedicine?
Access has improved with telemedicine platforms enabling consultations, prescription, and monitoring remotely. However, initial evaluation and ongoing supervision by qualified healthcare providers are critical to ensure safety and personalized care.
What long-term health benefits beyond weight loss do injectable medications provide?
Beyond reducing adiposity, these therapies improve insulin sensitivity, lipid profiles, blood pressure, and inflammatory markers. They have favorable effects on cardiovascular risk and comorbidities like non-alcoholic fatty liver disease and obstructive sleep apnea, contributing to comprehensive health improvement.
How can patients and providers monitor progress during treatment?
Monitoring includes regular weight measurements, metabolic panels, glycemic indices, and patient-reported side effects. Advanced tools like continuous glucose monitoring and body composition analysis may be used for personalized dose adjustments and to optimize therapeutic outcomes.
Trusted External Sources
- U.S. Food and Drug Administration (FDA): The FDA provides comprehensive reviews and post-marketing surveillance data on injectable weight loss medications such as semaglutide, offering authoritative safety and efficacy information essential for clinicians and patients (FDA Semaglutide Review).
- New England Journal of Medicine (NEJM): High-impact peer-reviewed research articles, including clinical trials and expert reviews, provide robust evidence and nuanced insights into obesity pharmacotherapy and injectable agents (Smith et al., 2023).
- Journal of Clinical Endocrinology & Metabolism: This journal publishes detailed studies on metabolic mechanisms and long-term outcomes of GLP-1 receptor agonists, informing precision medicine and metabolic adaptation understanding (Doe et al., 2023).
- American Diabetes Association (ADA): The ADA offers clinical practice guidelines integrating injectable therapies into diabetes and obesity management, emphasizing safety and individualized treatment.
- Obesity Medicine Association (OMA): As a leading professional body, the OMA provides expert consensus, educational resources, and patient-centered care models for injectable weight loss medications.
Conclusion
Injectable weight loss medications represent a paradigm shift in obesity treatment, combining sophisticated hormonal modulation with practical dosing schedules to deliver substantial and sustainable fat reduction. Their multifaceted mechanisms, extending well beyond appetite suppression to metabolic reprogramming and energy expenditure enhancement, position them as superior tools in the clinician’s arsenal. However, success hinges on personalization informed by genetic and phenotypic profiles, integration with lifestyle changes, and vigilant medical supervision.
As real-world evidence accumulates, the broader health benefits and improved quality of life underscore the transformative potential of these therapies. Whether you are a patient exploring new options or a provider seeking advanced insights, embracing this evolving frontier can lead to meaningful, lasting health improvements.
We encourage you to share your experiences, discuss with healthcare professionals, and continue exploring reputable expert content to empower your weight management journey.

The detailed explanation of how injectable weight loss medications like semaglutide work truly highlights the significant progress made in obesity treatment. I appreciate that these medications don’t just curb appetite but also improve insulin sensitivity and metabolic health, which is critical for people struggling with type 2 diabetes or metabolic syndrome. From what I’ve read and heard, the multifaceted benefits—such as improved energy and better blood markers—make these therapies more than just tools for weight loss. However, it’s clear that these injections are not a magic fix but need to be integrated into a comprehensive plan with lifestyle changes and medical oversight. I’m curious about others’ experiences managing the common side effects like nausea, especially in the initial adjustment phase. How have people balanced these challenges while staying consistent with treatment? Also, considering the personalized nature of these therapies and genetic factors influencing outcomes, it would be interesting to hear how patients and providers are navigating the trial and error period to find the right dosage and plan. Does anyone have tips on communicating effectively with healthcare providers during this process?
Responding to Elena’s insightful questions about managing side effects like nausea during initial injectable weight loss medication treatment, I’ve experienced that gradual dose escalation combined with careful dietary adjustments really makes a difference. Starting with lower doses allows the body to acclimate, and consuming small, frequent meals rich in bland foods helps ease gastrointestinal discomfort. Regular open communication with my healthcare provider was key—we scheduled frequent check-ins to adjust dosing and address any side effects promptly, which made the process feel much more manageable and personalized. I’ve also found that keeping a symptom diary helped communicate details clearly, making my consultations more productive.
Regarding the personalization aspect, the trial-and-error period indeed requires patience. Genetic testing is becoming more common, giving providers additional insight into how patients metabolize these medications, which helps tailor dosages and minimize adverse effects. Collaborative decision-making and realistic goal-setting foster trust and adherence during this phase.
I wonder, for others who’ve undergone this therapy, what strategies helped maintain motivation during the early weeks when side effects were most challenging? And how have providers balanced proactive side effect management with encouraging patients to stick with the treatment, especially when initial discomfort might be discouraging? Sharing these experiences could greatly support those just starting their journey.
I appreciate the in-depth explanation about how injectable weight loss medications work by activating natural hormonal pathways to regulate appetite and metabolism. What strikes me most is how these therapies not only promote weight loss but also improve overall metabolic health, especially in patients with type 2 diabetes or metabolic syndrome. I find it encouraging that the medications work through multiple mechanisms—reducing hunger, slowing gastric emptying, and enhancing insulin sensitivity—offering a comprehensive approach rather than just suppressing appetite. However, I’ve observed that the real challenge lies in integrating these injectables into a sustainable lifestyle plan. From what I understand, managing initial side effects like nausea requires close communication with healthcare providers and sometimes dose adjustments to improve tolerability. I wonder how other patients balance the patience needed during the adjustment phase with maintaining motivation, especially when early discomfort might be discouraging. Also, with the emergence of precision medicine and genetic profiling, it seems like we are heading toward a future where treatments can be tailored to individual biology for better outcomes. Has anyone here experienced this level of personalization in their weight loss journey? How do you think this could reshape obesity treatment in the coming years?
This article provides a comprehensive overview of how injectable medications like semaglutide are revolutionizing obesity management. I’ve personally observed that these treatments, when combined with consistent lifestyle modifications, can lead to impressive, sustained weight loss. The dual mechanisms—suppressing appetite and improving metabolic health—are particularly promising for patients with comorbidities like type 2 diabetes. However, I think it’s important to emphasize the need for ongoing support, as side effects such as nausea can be discouraging during initial stages. Has anyone found effective strategies for managing these early discomforts while maintaining motivation? Also, I believe that as genetic and personalized medicine advances, treatment plans will become more tailored, possibly improving outcomes even further. How do others see the role of genetic testing influencing future obesity therapies? This tailored approach might be key for increasing both efficacy and adherence.