Unlocking the Science Behind Prescription Weight Loss Medications
Prescription weight loss medications have revolutionized the approach to obesity and fat loss by integrating medical expertise with biological science. Unlike fad diets or unregulated supplements, these medications are designed to support healthy fat loss by targeting specific physiological pathways that regulate appetite, metabolism, and fat storage. This precision medicine approach not only enhances fat reduction but also promotes sustainable lifestyle changes, making them a powerful tool in comprehensive weight management.
Beyond Calories: How Medications Redefine Fat Loss Mechanisms
At the core of prescription weight loss drugs is their ability to modulate hormones and neural signals responsible for hunger and satiety. For instance, GLP-1 receptor agonists—such as semaglutide and tirzepatide—mimic the incretin hormones that enhance insulin secretion and delay gastric emptying. This results in reduced appetite and increased feelings of fullness, helping individuals naturally consume fewer calories without the struggle of constant hunger. Moreover, these medications improve metabolic efficiency by influencing fat oxidation processes, which supports healthier fat loss beyond simple calorie restriction.
Real-Life Impact: Case Scenarios Illustrating Medication Benefits
Consider Jane, a 45-year-old woman with obesity-related hypertension who struggled to lose weight despite diet and exercise. After starting a medically supervised regimen including prescription weight loss medication, she experienced a significant reduction in appetite and lost 15% of her body weight over six months. This not only improved her blood pressure but also enhanced her energy levels and psychological well-being. Such examples highlight how prescription medications, when combined with physician-led plans, can transform weight loss journeys into holistic health improvements.
How Do Prescription Weight Loss Medications Support Long-Term Healthy Fat Loss?
Prescription weight loss medications are most effective when integrated into a broader strategy emphasizing lifestyle modification, including nutrition, physical activity, and behavioral support. They help break the cycle of weight regain by addressing underlying metabolic and hormonal imbalances that often sabotage long-term success. By reducing hunger and improving metabolic parameters, these drugs create a physiological environment conducive to sustained fat loss. However, their role is supportive—not standalone—and optimal outcomes depend on adherence to medical guidance and lifestyle changes.
Choosing the Right Medication: Personalized Approaches for Optimal Results
Not all prescription weight loss drugs are suitable for everyone. Factors such as existing health conditions, medication side effects, and individual metabolic profiles guide physicians in selecting the safest and most effective option. This personalized approach maximizes fat loss while minimizing risks, aligning treatment with each patient’s unique needs. For those interested in exploring these options, resources like how to qualify for prescription weight loss medications offer detailed insights into eligibility and next steps.
Expert Insight: Trusting Science and Medical Oversight
It’s essential to rely on FDA-approved medications prescribed by healthcare professionals who monitor progress and adjust treatment plans accordingly. According to the National Institutes of Health, these medications have demonstrated efficacy and safety through rigorous clinical trials, underscoring their role in modern obesity management. This medical oversight ensures that fat loss is not only effective but also aligned with overall health and wellness goals.
If you’re considering prescription weight loss medications and want to explore personalized, doctor-led plans, feel free to contact a medical professional today to start your transformative journey.
My Experience Navigating Medication Choices
When I first started exploring prescription weight loss medications, I quickly realized how crucial personalized care is. Each person’s body responds differently, and what worked wonders for my friend didn’t suit me at all. The thoughtful guidance from my healthcare provider helped me avoid common pitfalls and choose a medication aligned with my health profile and lifestyle. This experience reinforced how essential medical oversight is—not just for safety but to tailor strategies that truly fit individual needs.
Integrating Medication with Lifestyle: The Real Game-Changer
One of the biggest lessons I learned is that prescription medications are a powerful support, but they shine brightest when coupled with meaningful lifestyle changes. I incorporated better nutrition habits and regular physical activity while on my prescribed treatment. The medications helped curb my appetite and boost my energy, making it easier to stay consistent. Over time, these combined efforts led to more sustainable fat loss and improved my overall well-being.
How Do You Balance Medication Benefits with Lifestyle Changes?
This question often comes up in discussions with others considering weight loss medications. Is it possible to rely solely on medication? From my perspective and supported by experts, the answer is no. Medications create a foundation by addressing biological barriers like excessive hunger or slow metabolism, but lasting results require commitment to healthier habits. It’s about creating synergy between medical tools and daily choices.
Trusting Science in Your Weight Loss Journey
I’ve found comfort in knowing that the medications I used are backed by extensive research, such as the findings shared by the National Institutes of Health. Their studies highlight not only the effectiveness of GLP-1 receptor agonists but also underscore the importance of physician supervision throughout treatment. This reassurance can make a big difference when embarking on what sometimes feels like a daunting journey.
What’s Next? Sharing and Learning Together
If you’ve tried prescription weight loss medications or are curious about starting, I’d love to hear your story or thoughts. Sharing experiences helps build a supportive community where we can learn what works and what to avoid. Feel free to comment below or explore related resources like doctor-prescribed weight loss plans to find strategies tailored for you.
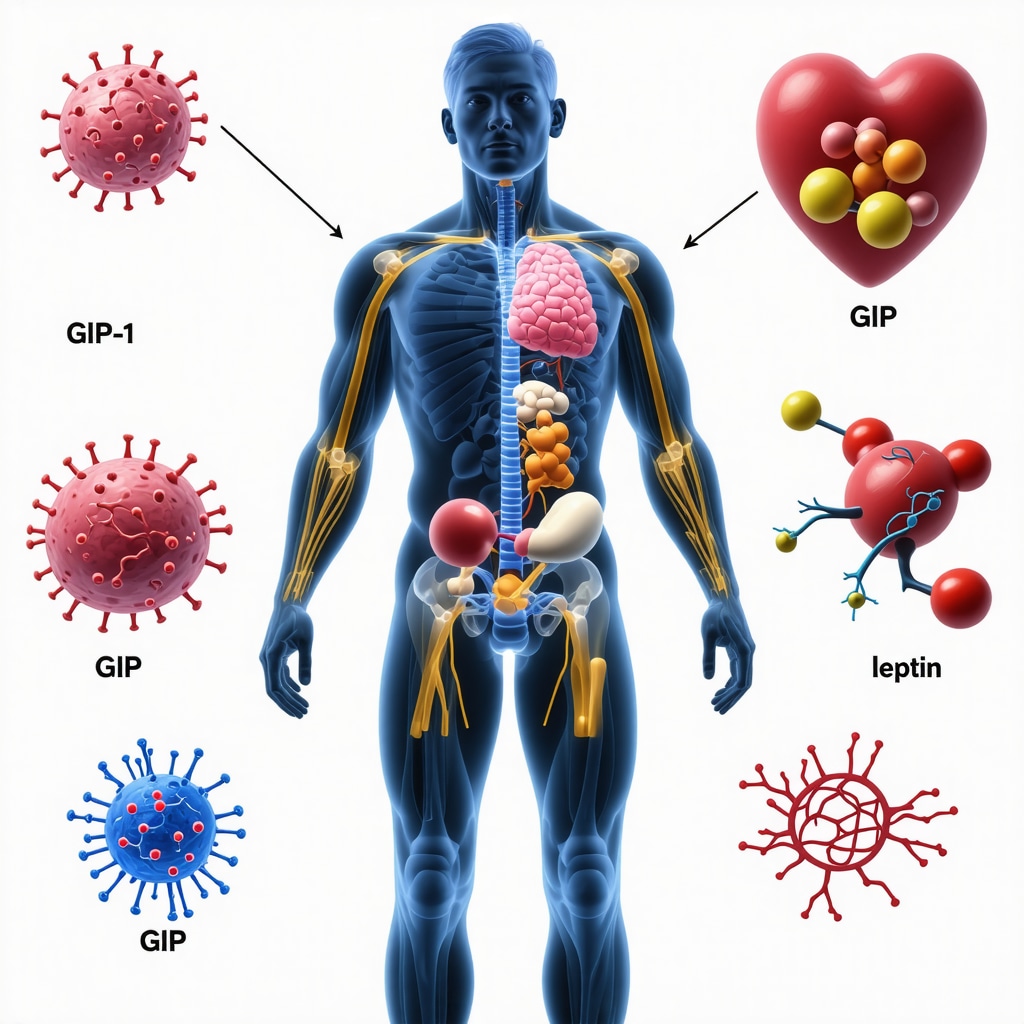
Decoding Metabolic Adaptation: Overcoming Plateaus with Prescription Medications
One of the most challenging aspects of sustainable fat loss is the body’s natural tendency toward metabolic adaptation, often manifesting as weight loss plateaus or rebounds. Prescription weight loss medications can play a pivotal role in mitigating these physiological defenses. By modulating appetite hormones such as ghrelin and leptin, and enhancing insulin sensitivity, these agents help counteract the metabolic slowdown that typically follows initial weight reduction. This nuanced interaction fosters a metabolic environment where continued fat oxidation is feasible, even when caloric intake is reduced.
Moreover, certain medications influence energy expenditure indirectly by improving mitochondrial function and promoting favorable shifts in adipose tissue biology. Such mechanisms transcend mere calorie counting, aiming instead to recalibrate the body’s energy homeostasis. This sophisticated approach helps patients maintain momentum in their weight loss journey, particularly those who have struggled with repeated plateaus despite rigorous lifestyle adherence.
How Do Prescription Weight Loss Medications Interact with Hormonal Feedback Loops to Sustain Fat Loss?
Prescription weight loss medications intricately interact with the body’s hormonal feedback systems responsible for hunger, satiety, and energy balance. For example, GLP-1 receptor agonists stimulate incretin hormones that enhance insulin secretion and suppress glucagon release, aiding glycemic control while promoting satiety. Additionally, they delay gastric emptying, which prolongs fullness and reduces postprandial glucose spikes.
Medications like bupropion-naltrexone target the central nervous system to modulate reward pathways and decrease food cravings, thus complementing peripheral mechanisms. These dual-action effects disrupt the usual counter-regulatory responses to weight loss, such as increased hunger and decreased energy expenditure, by recalibrating neuroendocrine circuits. This complex interplay is critical for sustaining fat loss over the long term and minimizing rebound weight gain.
Integrating Pharmacotherapy with Precision Nutrition and Exercise Prescription
Optimizing fat loss outcomes requires a multidisciplinary approach that synergizes prescription medications with personalized nutrition and exercise regimens. Precision nutrition, guided by metabolic phenotyping and genetic insights, allows tailoring macronutrient composition and meal timing to enhance medication efficacy. For instance, low-glycemic diets may amplify the benefits of GLP-1 receptor agonists by stabilizing blood glucose levels and reducing insulin resistance.
Exercise prescriptions should focus not only on caloric expenditure but also on improving mitochondrial density, enhancing lipid oxidation, and preserving lean muscle mass. Resistance training paired with aerobic conditioning can optimize body composition changes, augmenting the pharmacological effects on fat loss. Collaborative care involving dietitians, physiologists, and physicians ensures that interventions are harmonized and individualized for maximal impact.
Emerging Research: Novel Targets and Combination Therapies in Fat Loss Pharmacology
The landscape of prescription weight loss medications is rapidly evolving with novel agents targeting diverse metabolic pathways. Combination therapies that pair GLP-1 receptor agonists with agents affecting glucagon receptors or GIP (glucose-dependent insulinotropic polypeptide) receptors are showing promise in amplifying fat loss while mitigating side effects.
Additionally, advances in understanding brown adipose tissue activation and its role in thermogenesis open new avenues for pharmacological enhancement of energy expenditure. Early-phase clinical trials are investigating molecules that stimulate uncoupling proteins and promote browning of white adipose tissue, potentially revolutionizing fat loss strategies.
Integrating these innovative therapies into clinical practice will require rigorous evaluation and expert oversight but heralds a new era of precision obesity medicine.
For those eager to delve deeper into the cutting-edge science of fat loss medications and tailored weight management plans, consider consulting with specialists who prioritize a holistic, evidence-based approach. Reach out today to explore personalized strategies backed by the latest research.
Precision Hormonal Modulation: The Keystone of Sustained Fat Loss
In the realm of prescription weight loss medications, the intricate orchestration of hormonal pathways is paramount. These agents do not merely suppress appetite transiently; they recalibrate the neuroendocrine feedback loops governing energy homeostasis. By targeting hormones such as leptin, ghrelin, and incretins, medications like semaglutide profoundly influence hunger signaling and satiety perception, thereby fostering an environment conducive to long-term adipose tissue reduction.
What Are the Mechanistic Nuances Behind Medication-Induced Hormonal Feedback Disruption?
Prescription weight loss drugs intricately interface with the body’s hormonal milieu to disrupt compensatory responses that typically hinder sustained fat loss. For instance, GLP-1 receptor agonists enhance insulin secretion and inhibit glucagon release, improving glycemic control while prolonging gastric emptying to extend satiety. Concurrently, agents such as bupropion-naltrexone modulate central dopaminergic and opioid pathways, attenuating cravings by recalibrating reward circuits. This dual peripheral and central modulation attenuates the canonical increase in hunger and decrease in energy expenditure that follow weight loss, enabling more durable results.
Synergizing Pharmacotherapy with Metabolic Phenotyping for Tailored Interventions
Harnessing the full potential of prescription weight loss medications necessitates integration with precision medicine paradigms, including metabolic phenotyping and genomics. By characterizing individual variations in insulin sensitivity, adipose tissue distribution, and mitochondrial function, clinicians can customize pharmacological and lifestyle interventions to optimize efficacy. For example, patients exhibiting insulin resistance may benefit from GLP-1 receptor agonists coupled with low-glycemic diets, while those with specific genetic markers might respond preferentially to combination therapies targeting multiple hormonal axes.
This personalized approach not only maximizes fat loss but also mitigates adverse effects, enhancing adherence and overall patient satisfaction.
Cutting-Edge Developments: Exploring Polypharmacology and Thermogenic Modulators
Recent advances underscore the promise of polypharmacological agents that simultaneously target multiple receptors and pathways involved in energy regulation. The advent of triple agonists engaging GLP-1, GIP, and glucagon receptors exemplifies this evolution, demonstrating superior fat loss outcomes in preliminary clinical trials by leveraging synergistic metabolic effects.
Additionally, burgeoning research into pharmacological activation of brown adipose tissue (BAT) thermogenesis offers innovative avenues for enhancing basal energy expenditure. Agents that stimulate uncoupling protein 1 (UCP1) expression or promote browning of white adipose tissue could revolutionize obesity treatment by augmenting caloric dissipation through heat production.
Authoritative Perspective: National Institutes of Health on Emerging Therapeutics
According to a comprehensive review published by the National Institutes of Health, the integration of next-generation pharmacotherapies with lifestyle interventions represents a paradigm shift in obesity management. Their analysis emphasizes the necessity of multidisciplinary collaboration and continuous monitoring to optimize therapeutic outcomes while minimizing risks.
If you aspire to transcend conventional weight loss strategies and explore these advanced pharmacological options, consider consulting with specialists who pioneer evidence-based, individualized care.
Engage with expert clinicians today to unlock the transformative potential of personalized prescription weight loss therapies.
Frequently Asked Questions (FAQ)
What are prescription weight loss medications, and how do they differ from over-the-counter supplements?
Prescription weight loss medications are FDA-approved drugs designed to target specific physiological pathways involved in appetite regulation, metabolism, and fat storage. Unlike over-the-counter supplements, which often lack rigorous testing and regulatory oversight, these medications undergo extensive clinical trials to ensure safety, efficacy, and standardized dosing, making them a reliable component of medically supervised weight management.
How do GLP-1 receptor agonists help in fat loss?
GLP-1 receptor agonists mimic incretin hormones that enhance insulin secretion, delay gastric emptying, and promote satiety. This leads to reduced hunger and lower caloric intake, improved glycemic control, and increased fat oxidation. Their multifaceted hormonal effects support sustainable fat loss beyond simple calorie restriction.
Can prescription weight loss medications be used without lifestyle changes?
While these medications provide crucial physiological support by modulating appetite and metabolism, they are most effective when combined with lifestyle interventions such as balanced nutrition, physical activity, and behavioral counseling. Relying solely on medications without lifestyle changes typically limits long-term success and increases the risk of weight regain.
What factors influence the choice of a specific weight loss medication?
Physicians consider individual health profiles, including existing medical conditions, metabolic characteristics, potential side effects, and patient preferences. This personalized approach ensures maximum efficacy and safety, tailoring treatment plans to each patient’s unique needs.
How do prescription weight loss medications address metabolic adaptation and plateaus?
These medications interact with hormonal feedback loops involving ghrelin, leptin, and insulin, mitigating the body’s natural metabolic slowdown that often causes plateaus. By recalibrating hunger signals and enhancing energy expenditure through mechanisms like improved mitochondrial function, they help maintain continuous fat loss despite physiological defenses.
Are there emerging therapies that combine multiple mechanisms for enhanced fat loss?
Yes, novel combination therapies such as triple agonists targeting GLP-1, GIP, and glucagon receptors are under investigation. These agents leverage synergistic effects on metabolism and appetite regulation, showing promising results in preliminary trials for superior fat loss outcomes with manageable side effects.
How important is medical supervision during medication-assisted weight loss?
Medical supervision is critical to monitor efficacy, manage side effects, adjust dosages, and integrate medications with comprehensive lifestyle strategies. Healthcare professionals ensure safety and optimize personalized treatment, enhancing adherence and long-term success.
Can pharmacological activation of brown adipose tissue aid fat loss?
Emerging research suggests that stimulating brown adipose tissue (BAT) thermogenesis can increase basal energy expenditure by converting calories into heat. Pharmacological agents promoting BAT activation or browning of white adipose tissue hold potential to augment fat loss, though these therapies are still under clinical evaluation.
How does precision nutrition complement prescription weight loss medications?
Precision nutrition involves tailoring dietary plans based on metabolic phenotyping and genetic factors to optimize medication effects. For example, low-glycemic diets may enhance the benefits of GLP-1 receptor agonists by stabilizing blood glucose and reducing insulin resistance, thereby improving fat loss outcomes.
What role does exercise play alongside prescription weight loss drugs?
Exercise complements pharmacotherapy by increasing energy expenditure, enhancing mitochondrial density, preserving lean muscle mass, and improving lipid oxidation. A balanced regimen combining resistance training and aerobic conditioning synergizes with medications to maximize fat loss and improve overall metabolic health.
Trusted External Sources
- National Institutes of Health (NIH) – Provides comprehensive reviews and clinical trial data on obesity pharmacotherapy, offering authoritative evidence on the efficacy and safety of prescription weight loss medications.
- Endocrine Society Clinical Practice Guidelines – Offers expert consensus on obesity management, including detailed recommendations for the use of weight loss drugs and integration with lifestyle interventions.
- American Diabetes Association (ADA) – Publishes research on incretin-based therapies like GLP-1 receptor agonists, elucidating their mechanisms and clinical implications in metabolic disorders and weight management.
- Obesity Society – A leading organization dedicated to obesity research, providing access to cutting-edge studies and expert position statements on pharmacological treatments.
- Journal of Clinical Endocrinology & Metabolism (JCEM) – A peer-reviewed journal featuring seminal research articles on hormonal regulation, metabolic adaptation, and novel pharmacotherapies in obesity.
Conclusion
Prescription weight loss medications represent a transformative advancement in obesity management by precisely modulating hormonal and metabolic pathways that govern hunger, satiety, and energy balance. Their efficacy is maximized when integrated with individualized lifestyle interventions, including precision nutrition and tailored exercise regimens, under vigilant medical supervision. Emerging therapies that harness polypharmacology and thermogenic mechanisms promise to further enhance sustainable fat loss outcomes. By embracing a multifaceted, evidence-based approach, patients can overcome metabolic adaptation challenges and achieve durable, healthy weight reduction. If you’re ready to explore personalized strategies that combine science-driven pharmacotherapy with holistic care, consider consulting healthcare professionals who specialize in precision obesity medicine. Share your experiences, ask questions, and continue learning to empower your weight loss journey with knowledge and expert guidance.

Reading about how prescription weight loss medications like GLP-1 receptor agonists actually engage with our body’s hormonal pathways to reduce hunger and improve metabolism is really eye-opening. It’s a relief to see that these aren’t just quick fixes, but tools that work in tandem with sustainable lifestyle changes. From my perspective, the most challenging part is maintaining those lifestyle changes long-term once the initial medication support tapers off. For example, I’ve noticed in some people that after stopping medication, the signals for hunger and satiety can become confusing again, making them prone to regain weight.
I appreciate how the post highlights the necessity of personalized medical supervision; it reinforces that weight management isn’t one-size-fits-all. I’m curious how others have balanced the transition off medications while keeping the healthy habits intact. Have anyone found specific strategies or support systems that help ease this shift? Also, how do clinicians typically help patients prepare for potential metabolic adaptation during or after medication use? It would be great to hear personal experiences or professional approaches to this aspect of long-term weight loss.
Eleanor, your observation about the challenges of maintaining lifestyle changes after tapering off prescription weight loss medications really resonates with what I’ve learned. From what I’ve gathered, many clinicians emphasize a gradual transition plan, which includes ongoing behavioral therapy and nutritional counseling to reinforce habits formed during medication use. Regular follow-ups to monitor metabolic markers and appetite cues seem crucial to catch early signs of weight regain or metabolic adaptation. Some healthcare providers also incorporate adaptive exercise programs that evolve as patients reduce their medication dosage, aiming to sustain increased energy expenditure.
Personally, I’ve seen that building a robust support network—whether through group counseling or digital health coaching—plays a pivotal role in sustaining the gains after stopping medication. This kind of social accountability can help navigate confusing hunger and satiety signals that might return.
Given that metabolic adaptation is such a complex process involving hormonal feedback loops, how do others here balance patience and persistence with modifying their plans? Are there particular strategies or tools that have helped recalibrate your body’s responses when medication phases out? Sharing how experienced clinicians tailor these long-term plans would be insightful for all of us navigating this important phase.
This post really underscores how crucial personalized treatment plans are when it comes to prescription weight loss meds. I’ve seen firsthand how GLP-1 receptor agonists like semaglutide can be powerful tools for reducing appetite, but they’re just one part of a bigger picture. From my own experience, long-term success depends heavily on ongoing behavioral support and adapting lifestyle habits, especially once medication support begins to taper. It’s interesting that the hormonal pathways are so intricate – it makes me wonder, how do clinicians best assess when a patient is ready to slowly reduce medication while minimizing the risk of rebound hunger or weight regain?
Also, I’d love to hear more about integrating emerging research on brown adipose tissue activation with everyday weight management. Has anyone here explored approaches beyond medications, like targeted nutrition or specific exercise regimens, to boost energy expenditure naturally?
Balancing medication use with sustainable habits is definitely a puzzle, but with continued research and tailored care, it seems possible to create a durable strategy for fat loss. What are some of the most effective tools or mindset shifts you’ve used to maintain motivation and adherence during long-term weight management? Looking forward to everyone’s insights.
This post really emphasizes the science-backed approach to weight loss medications and how they can offer real support when integrated properly into a holistic plan. I’ve personally seen how GLP-1 receptor agonists like semaglutide can significantly reduce appetite, especially during the initial phases of treatment. However, I believe one challenge that often gets overlooked is how to maintain motivation long-term once medications are tapered or discontinued. It seems crucial to develop a robust support system that includes behavioral, nutritional, and exercise strategies that adapt alongside medication use.
I also wonder, with the rapid advancements in targeting brown adipose tissue activation and thermogenesis, how soon we might see these options become part of standard treatment protocols? Could combining pharmacotherapy with targeted energy expenditure strategies lead to even more sustainable weight management outcomes? I’d be eager to hear from anyone experimenting with or considering multi-modal approaches that go beyond conventional medications.