Why Doctor-Led Fat Loss Plans Are Revolutionizing Weight Management
In the complex landscape of weight loss, cookie-cutter programs often fall short. Doctor-led fat loss plans stand apart by weaving medical expertise into personalized strategies that address your unique biology, lifestyle, and health conditions. Unlike generic diets, these programs integrate evidence-based approaches crafted by physicians who understand the intricacies of metabolism, hormonal balance, and chronic disease management. This tailored precision transforms fat loss from a frustrating guessing game into a scientifically guided journey with measurable results.
Personalized Programs: The Intersection of Medicine and Metabolic Mastery
Medical supervision in fat loss means comprehensive assessment—blood markers, body composition, and metabolic rate—inform every step. Doctors can identify underlying issues such as insulin resistance or thyroid dysfunction that sabotage traditional efforts. Incorporating prescription weight loss medications, like GLP-1 receptor agonists, under physician guidance optimizes fat burning safely. This medical approach ensures that interventions are not only effective but also sustainable, minimizing side effects and maximizing long-term adherence.
How Do Doctor-Led Fat Loss Plans Differ from Standard Diets and Fitness Regimens?
While general diets and exercise plans promote broad calorie deficits and physical activity, doctor-led fat loss plans delve deeper. They customize macronutrient ratios, medication protocols, and behavioral modifications based on thorough medical evaluation. This nuanced strategy acknowledges that weight loss is not one-size-fits-all but a multifactorial challenge requiring targeted solutions. For instance, a patient with metabolic syndrome may receive a distinct program emphasizing insulin sensitivity improvements alongside lifestyle changes, a precision that typical plans lack.
Real-World Success: Case Studies Illuminating Medical Weight Loss Excellence
Consider Jane, a 45-year-old with a history of failed diets and hypothyroidism. Under a doctor-led fat loss plan, her medication regimen was optimized alongside a personalized nutritional plan. Over six months, Jane lost 30 pounds, improved her thyroid function, and reported enhanced energy and mood. This exemplifies the power of integrating medical insight with individualized programming—transformations grounded in science, not fad.
Exploring Cutting-Edge Treatments Within Doctor-Guided Fat Loss Programs
Advancements such as GLP-1 receptor agonists and semaglutide versus tirzepatide therapies exemplify how physician-guided interventions can harness pharmacology alongside lifestyle modification. These FDA-approved treatments, when prescribed judiciously, amplify fat loss efficacy while offering safety profiles vetted through rigorous clinical trials. The expertise of a physician ensures that patients receive the right drug, dose, and monitoring tailored to their health status.
Integrating Lifestyle and Medical Insight for Sustainable Fat Loss
A hallmark of doctor-led programs is the holistic focus on sustainable behavior change. Medical supervision facilitates not only physiological adjustments but also psychological support, addressing emotional eating, motivation, and adherence challenges. This comprehensive model empowers patients with tools and knowledge, fostering long-term success beyond the initial weight loss phase.
Ready to Experience a Doctor-Led Fat Loss Plan Tailored Just for You?
If you’ve struggled with generic diets or need a medically supervised, personalized program that truly delivers, exploring a doctor-guided fat loss plan could be transformative. Visit this resource to learn how physician expertise combines with cutting-edge science for real results. Share your experiences or questions in the comments below to join a community committed to effective, safe fat loss.
For further authoritative insight, the National Institutes of Health offers extensive research on the efficacy of medically supervised weight loss interventions, underscoring the benefits of physician involvement in obesity management.
When the Journey Gets Tough: Overcoming Plateaus and Setbacks
Embarking on a doctor-led fat loss plan doesn’t mean the path will always be smooth. I’ve encountered my fair share of plateaus where the scale refused to budge despite sticking to the program perfectly. What helped me push through was maintaining open communication with my healthcare provider to adjust medications or tweak nutritional plans based on updated lab results and real-time feedback. This dynamic approach allowed me to personalize my journey even further and avoid frustration.
Understanding that plateaus are often a natural biological response rather than failure is crucial. For instance, metabolic adaptations can slow weight loss temporarily. Incorporating small changes like varying exercise routines or revisiting meal timing under medical guidance helped me overcome these stalls more effectively than generic advice ever could.
The Crucial Role of Mental Health Support in Medical Fat Loss Programs
One aspect that surprised me was how deeply intertwined mental health and weight loss are. Doctor-led programs don’t just focus on the physical side but also provide psychological support, whether through counseling, stress management techniques, or behavioral therapy. Personally, acknowledging emotional eating triggers and working through them with professional help was a game changer in sustaining my fat loss.
It’s important to remember that the emotional journey is as significant as the physical. According to a study published by the National Institutes of Health, incorporating behavioral therapy alongside medical interventions improves long-term weight management outcomes significantly. This holistic approach helped me stay motivated and resilient.
How Can You Stay Motivated When Progress Feels Slow?
From my experience, setting small, achievable goals and celebrating non-scale victories—like improved energy levels, better sleep, or enhanced mood—can dramatically shift your mindset. Tracking progress through various metrics beyond weight, such as body composition or fitness milestones, provides tangible proof of your hard work paying off.
Also, engaging with a community or support group, either in person or online, encourages accountability and shared encouragement. If you’re interested, exploring resources like doctor-led fat loss plans can connect you with professionals who tailor strategies uniquely suited to your needs.
Practical Tips for Integrating Doctor-Led Plans into Your Daily Life
One challenge I faced was seamlessly incorporating medical recommendations into my busy routine. Here are some tips that worked well for me:
- Schedule regular check-ins: Make appointments consistent to allow for timely adjustments in your plan.
- Prepare meals ahead: Meal prepping based on your prescribed nutritional guidelines saved me from impulsive eating.
- Use medication reminders: Setting alarms or using apps ensured I never missed doses.
- Stay curious and informed: Reading trusted sources like GLP-1 medication guides helped me understand how treatments work and empowered me to ask better questions.
Integrating these small habits made the medical plan a natural part of my lifestyle rather than a disruptive obligation.
Have you tried a doctor-led fat loss program or are you considering one? Share your thoughts or personal stories in the comments below—your experience might inspire or help someone else on their journey. For those curious about the variety of FDA-approved options and how they can be safely integrated, I recommend exploring resources on safe prescription weight loss drugs and physician-guided plans tailored for success.
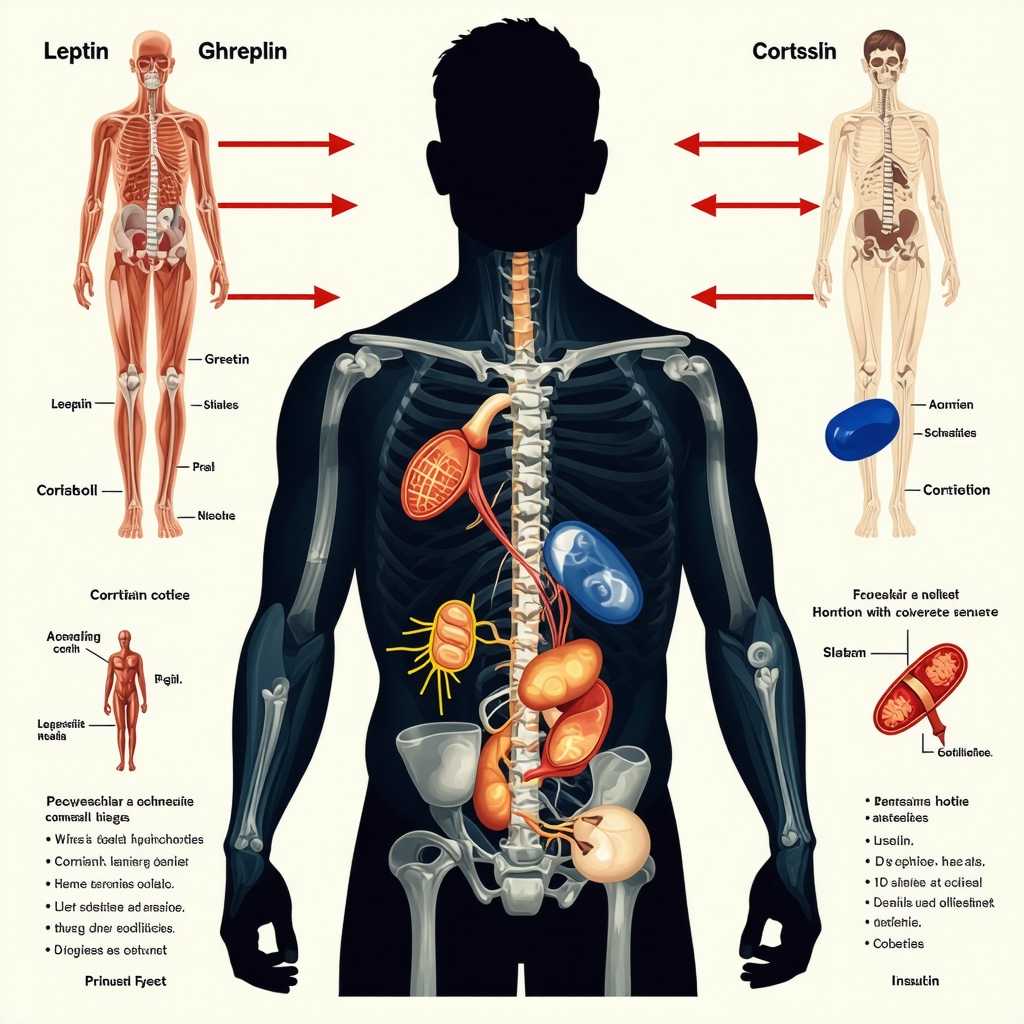
Decoding Hormonal Influences: The Hidden Drivers of Fat Loss Resistance
While calorie management remains a cornerstone of weight reduction, the hormonal landscape profoundly influences fat loss success, often dictating the ease or difficulty of shedding pounds. Hormones such as leptin, ghrelin, cortisol, and insulin orchestrate appetite regulation, fat storage, and energy expenditure in complex feedback loops. Doctor-led fat loss plans excel by employing targeted diagnostics to identify hormonal imbalances that hinder progress.
For example, elevated cortisol levels due to chronic stress can promote visceral fat accumulation and insulin resistance, creating metabolic roadblocks. Physicians may integrate stress management protocols, adapt medication regimens, or suggest specific nutritional adjustments that modulate cortisol secretion. Likewise, thyroid hormone deficiencies can blunt basal metabolic rate; tailoring thyroid hormone therapy alongside dietary optimization revitalizes metabolic function, accelerating fat loss.
How Do Doctor-Led Programs Tailor Interventions Based on Hormonal Profiles?
By leveraging comprehensive lab panels and clinical evaluations, doctors pinpoint hormonal disruptions that standard diets overlook. These insights allow for bespoke interventions: adjusting macronutrient ratios to improve insulin sensitivity, prescribing medications that influence appetite hormones, or implementing chrono-nutrition strategies aligning meal timing with circadian rhythms. This precision medicine approach transcends generic guidelines, accommodating the unique endocrine milieu of each patient.
Harnessing Metabolic Flexibility: Beyond Calorie Counting
Metabolic flexibility—the body’s capacity to efficiently switch between fuel sources like carbohydrates and fats—is a pivotal yet often under-addressed factor in sustained fat loss. Impaired metabolic flexibility can stall weight loss despite adherence to calorie deficits. Doctor-led plans often incorporate metabolic testing tools, such as indirect calorimetry, to assess substrate utilization patterns in real-time.
With these insights, physicians customize interventions to enhance mitochondrial function and fuel partitioning. Strategies may include targeted fasting windows, macronutrient cycling, or personalized exercise prescriptions emphasizing aerobic and resistance training balance. Such tailored regimens recalibrate metabolism, facilitating breakthrough from plateaus that stump conventional approaches.
The Role of Advanced Pharmacotherapy: Combining Efficacy with Safety
Beyond GLP-1 receptor agonists, emerging pharmacotherapies like combination agents and novel peptide analogs are expanding the therapeutic arsenal for fat loss. Doctor-led plans stay at the forefront by integrating these treatments judiciously, balancing efficacy with patient-specific risk profiles.
For instance, dual agonists that target multiple pathways involved in appetite and metabolism demonstrate superior weight loss outcomes in clinical trials. However, their use requires vigilant monitoring for adverse effects and contraindications, underscoring the indispensability of physician oversight. This ensures that each pharmacologic tool is deployed optimally within a holistic, medically supervised framework.
Optimizing Nutrigenomics: Personalizing Diet at the Genetic Level
The burgeoning field of nutrigenomics reveals how genetic variations impact nutrient metabolism and dietary response, offering another layer of personalization in doctor-led fat loss plans. By analyzing patients’ genetic markers, physicians can recommend diets that align with individual metabolic tendencies, such as varying carbohydrate tolerance or lipid processing efficiency.
Integrating nutrigenomic data enhances adherence and efficacy, as patients receive nutrition plans scientifically tailored to their DNA blueprint rather than generic advice. This cutting-edge approach exemplifies the evolution of medical weight loss from empirical to precision science.
For those intrigued by the integration of genetics and metabolism in weight management, the National Library of Medicine’s comprehensive review on nutrigenomics and obesity elucidates these concepts with clinical relevance.
What Are the Key Genetic Markers That Influence Fat Loss Success?
Genetic variants in genes such as FTO, MC4R, and PPARG have been linked to appetite regulation, fat storage, and insulin sensitivity. Doctor-led programs interpret these markers to personalize dietary macronutrients and lifestyle interventions, leveraging genetic insights to overcome biological barriers to weight loss.
Invitation to Deepen Your Journey: Engage with Expert-Led, Science-Backed Weight Loss
Understanding and manipulating the intricate interplay of hormones, metabolism, pharmacology, and genetics demands expert guidance. If you’ve found traditional diets insufficient or want to explore advanced, medically supervised fat loss strategies, I encourage you to delve into specialized doctor-led programs that harness these multifaceted insights.
Explore detailed resources and professional consultations at Doctor-Led Fat Loss Plans to take your weight management to a profoundly personalized and effective level. Share your questions or experiences below to join a community prioritizing evidence-based, expert-driven fat loss.
Decoding the Microbiome’s Influence on Fat Loss Dynamics
Emerging research highlights the gut microbiome as a pivotal yet often overlooked player in fat loss efficacy. Variations in gut bacterial composition can influence energy harvest, inflammation, and metabolic signaling pathways, directly affecting weight regulation. Doctor-led fat loss plans are increasingly incorporating microbiome profiling to identify dysbiosis and recommend personalized probiotics, prebiotics, or dietary modifications that restore microbial balance and enhance metabolic health.
Can Modulating the Gut Microbiota Improve Weight Loss Outcomes in Medically Supervised Programs?
Clinical studies indicate that specific strains such as Akkermansia muciniphila and Bifidobacterium species correlate with improved insulin sensitivity and reduced adiposity. By integrating microbiome analysis, physicians tailor interventions targeting these beneficial microbes through diet or supplementation, amplifying fat loss beyond traditional methods. This frontier of metabolic medicine exemplifies the sophistication of doctor-guided approaches over generic weight loss protocols.
Leveraging Digital Health Technologies to Enhance Doctor-Led Fat Loss Interventions
The integration of wearable devices, telemedicine, and AI-driven analytics empowers patients and clinicians alike to monitor physiological parameters continuously and adjust treatment plans dynamically. Real-time data on glucose trends, heart rate variability, and activity levels allow for precision tuning of nutritional and pharmacologic interventions, ensuring maximum efficacy and safety.
Such digital health ecosystems facilitate adherence through personalized feedback loops and behavioral nudges, transforming passive patients into active participants—a critical factor in overcoming common barriers in weight management.
Addressing the Challenge of Sarcopenic Obesity Within Medical Fat Loss Frameworks
Sarcopenic obesity, characterized by concurrent loss of muscle mass and excess fat, presents unique therapeutic challenges requiring nuanced management. Doctor-led plans incorporate resistance training protocols, protein optimization, and anabolic agents when appropriate to preserve lean mass while promoting fat reduction. This dual focus mitigates risks of frailty and metabolic dysfunction often overlooked in standard programs.
Understanding Inflammatory Pathways: A Medical Perspective on Chronic Low-Grade Inflammation and Fat Loss Resistance
Chronic low-grade inflammation is a well-documented impediment to effective fat loss, contributing to insulin resistance and altered adipose tissue function. Physician-guided interventions may include anti-inflammatory dietary patterns rich in omega-3 fatty acids, polyphenols, and fiber, alongside pharmacologic agents targeting inflammatory cytokines. This integrative approach addresses the root inflammatory milieu, thereby enhancing metabolic responsiveness.
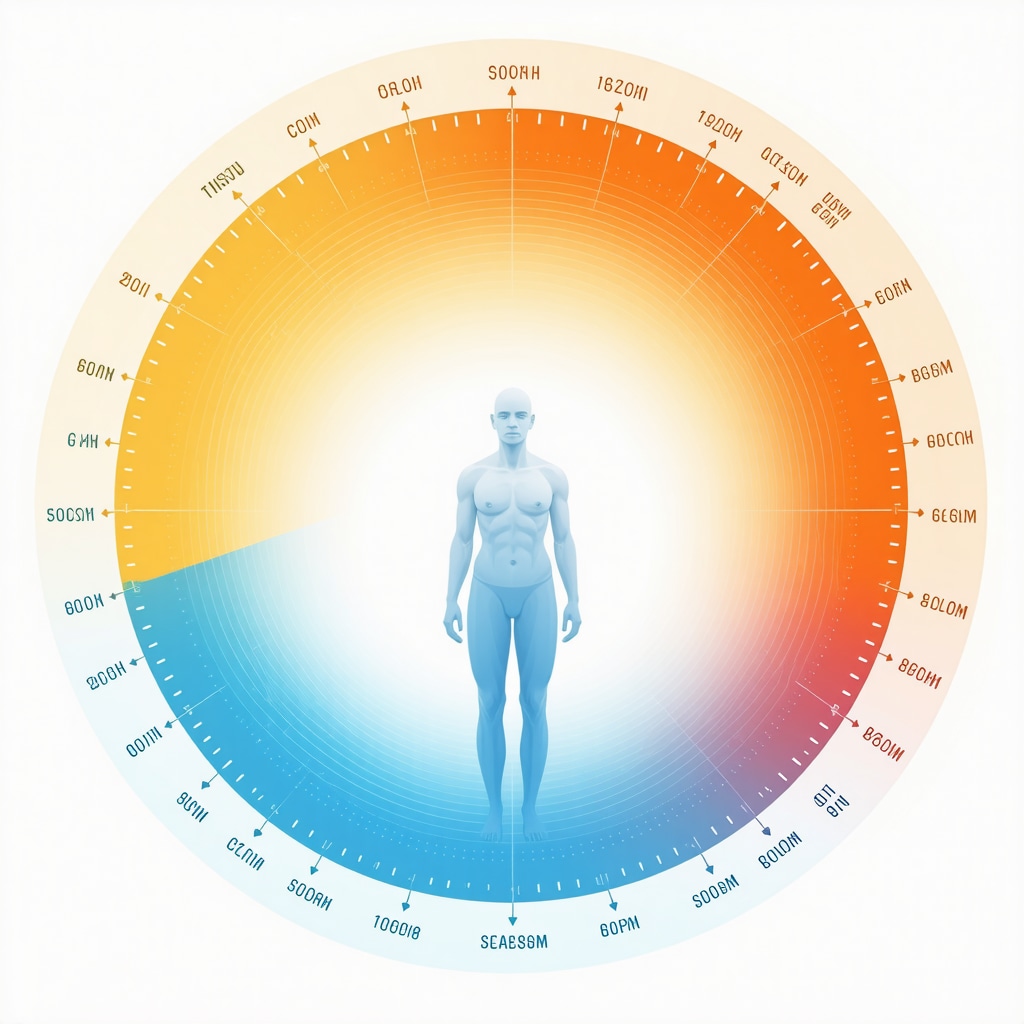
Exploring the Role of Circadian Biology in Optimizing Fat Loss Timing
Chronobiology research reveals that aligning eating and activity patterns with the body’s circadian rhythms can significantly impact metabolic outcomes. Doctor-led plans now often incorporate chrono-nutrition principles, recommending meal timing that synchronizes with hormonal fluctuations such as cortisol and insulin to maximize fat oxidation and minimize fat storage.
This temporal precision represents an advanced layer of personalization that transcends calorie counting, harnessing the body’s innate biological clock to optimize weight loss.
How Do Doctor-Led Fat Loss Plans Integrate Circadian Rhythm Insights to Enhance Metabolic Efficiency?
By assessing individual chronotypes and hormonal profiles, physicians prescribe meal schedules and exercise timing that capitalize on peak metabolic windows. For example, front-loading calories earlier in the day or implementing time-restricted feeding aligned with daylight hours can improve insulin sensitivity and lipid metabolism. This strategy reduces metabolic stress and supports sustained fat loss, illustrating the cutting-edge sophistication of medical weight management.
For an authoritative exploration of circadian rhythms in metabolism, consult the National Library of Medicine’s review on circadian regulation of metabolism, which underscores the clinical relevance of chronobiology in obesity treatment.
Invitation to Engage with Advanced, Evidence-Based Fat Loss Solutions
As the science of fat loss evolves, embracing multifactorial, medically supervised strategies becomes imperative for those seeking transformative results. If you are ready to transcend conventional dieting and leverage cutting-edge insights from genetics, microbiome, chronobiology, and digital health, explore specialized doctor-led programs designed for precision and sustainability.
Visit Doctor-Led Fat Loss Plans to connect with experts who will tailor an integrative approach uniquely suited to your physiological and lifestyle needs. Share your experiences or questions below to join a community committed to pioneering, science-driven weight management.
Frequently Asked Questions (FAQ)
What makes doctor-led fat loss plans more effective than typical diet and exercise programs?
Doctor-led plans leverage comprehensive medical assessments, including hormonal profiling and metabolic testing, to tailor interventions precisely to an individual’s physiology. This medical supervision allows for integration of evidence-based pharmacotherapy, behavioral therapy, and nutritional adjustments that address underlying causes of weight gain or resistance, resulting in more sustainable and measurable fat loss compared to generic approaches.
How do hormonal imbalances affect fat loss, and how are they managed in medical programs?
Hormones such as insulin, cortisol, thyroid hormones, leptin, and ghrelin regulate appetite, metabolism, and fat storage. Imbalances can slow fat loss or cause resistance. Doctor-led plans use targeted diagnostics to identify these disruptions and implement personalized treatments—ranging from medication adjustments to stress management and nutrition optimization—to restore hormonal balance and enhance fat loss efficacy.
Can genetic testing really influence weight loss strategies?
Yes. Nutrigenomics examines how genetic variants affect metabolism and nutrient processing. By analyzing specific markers like FTO or MC4R, physicians can recommend diets and lifestyle modifications aligned with a patient’s genetic predispositions, improving adherence and outcomes. This precision approach moves beyond one-size-fits-all dieting to scientifically guided personalization.
What role does the gut microbiome play in fat loss, and can it be modified for better results?
The gut microbiome influences energy extraction, inflammation, and metabolic signaling, all of which affect fat loss. Doctor-led programs may include microbiome profiling to detect imbalances and recommend targeted probiotics, prebiotics, or dietary changes to foster beneficial bacteria, thereby improving insulin sensitivity and reducing adiposity as part of an integrative treatment plan.
How do doctor-led plans address weight loss plateaus?
Plateaus often result from metabolic adaptations or hormonal shifts. These programs utilize ongoing monitoring and dynamic adjustments, such as modifying medication dosages, altering macronutrient ratios, incorporating varied exercise regimens, or adjusting meal timing based on circadian biology. This responsive approach helps overcome stagnation more effectively than static plans.
Are advanced weight loss medications safe, and how are they integrated into treatment?
FDA-approved medications like GLP-1 receptor agonists and emerging dual agonists have demonstrated safety and efficacy in clinical trials. Doctor supervision ensures appropriate patient selection, dosing, and monitoring for side effects or contraindications, integrating pharmacotherapy with lifestyle changes to maximize benefits safely.
Why is mental health support important in medically supervised fat loss?
Mental health significantly impacts motivation, adherence, and behaviors such as emotional eating. Doctor-led plans often incorporate psychological support, including counseling or behavioral therapy, to address these factors. This holistic care improves resilience and long-term success beyond physical interventions alone.
How can digital health tools enhance a doctor-led fat loss program?
Wearables, telemedicine, and AI-driven analytics provide continuous monitoring of physiological and behavioral data. This real-time feedback enables precise adjustments, promotes accountability, and supports personalized coaching, increasing engagement and treatment efficacy within medically supervised frameworks.
What strategies do doctor-led plans use to preserve muscle while losing fat, especially in sarcopenic obesity?
These programs emphasize resistance training, protein intake optimization, and may include anabolic agents when appropriate to maintain or increase lean muscle mass while reducing fat. Preserving muscle is critical to metabolic health and functional capacity, particularly in older adults or those with sarcopenic obesity.
How does circadian rhythm alignment improve fat loss outcomes?
Aligning meal timing and physical activity with natural circadian rhythms optimizes hormone secretion and metabolic processes that regulate fat oxidation and storage. Doctor-guided chrono-nutrition strategies customize schedules based on individual chronotypes and hormonal profiles, enhancing metabolic efficiency and weight loss sustainability.
Trusted External Sources
- National Institutes of Health (NIH) – Provides extensive peer-reviewed research on medically supervised weight loss interventions, hormone regulation, and behavioral therapies, underpinning evidence-based practices in doctor-led fat loss plans.
- National Library of Medicine (NLM) – Offers comprehensive reviews on emerging fields such as nutrigenomics, circadian biology, and microbiome influences in metabolism and obesity, supporting the scientific foundation for personalized medical weight management.
- Obesity Medicine Association (OMA) – A leading professional body specializing in obesity treatment guidelines, pharmacotherapy updates, and clinical best practices, ensuring doctor-led programs remain current with cutting-edge therapies.
- The American Journal of Clinical Nutrition (AJCN) – Publishes high-quality research on nutrition, metabolism, and weight management strategies critical to formulating precise dietary interventions in medical fat loss plans.
- Endocrine Society – Provides authoritative resources on hormone-related disorders and their impact on metabolism and obesity, guiding clinical assessment and treatment within physician-supervised weight loss frameworks.
Conclusion: Synthesizing the Science and Strategy of Doctor-Led Fat Loss
Doctor-led fat loss plans represent a transformative evolution in weight management, transcending simplistic calorie counting by integrating deep medical insight into the biological, genetic, and behavioral drivers of fat accumulation and resistance. Through personalized diagnostics, advanced pharmacotherapy, metabolic optimization, and psychosocial support, these programs tailor interventions uniquely to each patient’s physiology and lifestyle. This precision approach addresses root causes rather than symptoms, enabling sustainable, scientifically grounded fat loss with improved health outcomes.
As obesity and metabolic disorders grow increasingly complex, embracing multifaceted, evidence-based strategies under physician guidance is essential for real, lasting success. Whether tackling hormonal imbalances, leveraging nutrigenomics, or harnessing digital health innovations, doctor-led fat loss plans offer a comprehensive roadmap for those seeking to reclaim control over their weight and wellbeing.
Ready to elevate your weight loss journey with expert-driven, personalized care? Explore doctor-led programs, engage with the community, and apply these advanced insights to unlock your full fat loss potential. Share your questions or experiences below and join a movement towards smarter, safer, and more effective weight management.

What stood out to me in this post is how doctor-led fat loss plans really personalize every aspect of weight management—right down to hormonal balances and underlying health conditions, which are often overlooked in typical diet plans. As someone who has struggled with unexplained weight plateaus despite consistent dieting and exercise, learning that factors like thyroid dysfunction or insulin resistance could be silently sabotaging progress makes a lot of sense. The integration of medical assessments and prescription medications like GLP-1 receptor agonists under medical supervision offers a more tailored and potentially more sustainable option for individuals who haven’t found success with generic programs.
I also appreciate the mention of mental health support, which is crucial but often neglected. Emotional eating and motivation are huge hurdles for weight loss maintenance, and having psychological support integrated into these plans could be a game changer.
I’m curious how others have experienced the balance between medical interventions and lifestyle changes in these programs—specifically, how manageable do people find the integration of medications and personalized nutrition in daily life? Also, for those who have tried such plans, how was the communication with your doctor in terms of adjustments and staying motivated through challenges like plateaus? Would love to hear about real-life experiences with this comprehensive approach to weight loss!
I appreciate the comprehensive approach doctor-led fat loss plans take when managing weight loss, especially in recognizing that it’s not just about calories in and out but about addressing one’s unique biology. From my observation, what really sets these programs apart is the medical supervision that evaluates blood markers and metabolic rates, pinpointing issues like insulin resistance which often derail conventional diets. This level of precision seems crucial for lasting results.
One aspect that struck me was the integration of advanced treatments, such as GLP-1 receptor agonists, under physicians’ careful monitoring. These medications can be game changers if used appropriately, offering support beyond lifestyle modifications alone. It also feels important that these plans offer psychological and behavioral support, as motivation and emotional eating are critical factors often underestimated.
Considering all this, how have others found the balance between medical guidance and their daily routines? Are there particular strategies that helped you seamlessly incorporate prescribed medications and personalized nutrition into busy lifestyles? Additionally, how do you maintain open communication with your doctor to adapt your program as needed, especially when encountering plateaus? It would be enlightening to hear methods that have helped others stay engaged, motivated, and aligned with their health goals throughout this personalized journey.
The integration of medical expertise into fat loss plans, as detailed in this post, really highlights why one-size-fits-all diets often fail. I’ve always been skeptical of generic diet plans precisely because they don’t account for individual health complexities like hormonal imbalances or metabolic issues. This doctor-led approach, with its comprehensive assessments and personalized interventions, seems to offer a more science-backed and tailored route to weight loss.
What I find particularly compelling is how these plans address not only the physical but also the psychological aspects of weight management. Emotional eating and motivation barriers can seriously undermine progress, and having structured mental health support alongside medical treatment seems like a powerful combination for sustainable results.
I’m curious about the patient experience in terms of the balance between medical oversight and personal autonomy. For example, how flexible are these programs in adapting to lifestyle changes or patient feedback over time? Also, for anyone who has undergone such a plan, how has the integration of prescription medications influenced your day-to-day routine and adherence? Lastly, the mention of circadian rhythm-based meal timing piqued my interest—have others noticed tangible differences when aligning eating schedules with these biological rhythms?
It would be great to hear from readers about practical strategies that helped you merge these medical recommendations with your daily life and maintain motivation on tougher days.
This post truly sheds light on why doctor-led fat loss plans are changing the weight management landscape. What struck me most is how these programs don’t just focus on reducing calories or increasing activity, but instead dig into the biological and medical factors that often hinder success, such as hormonal imbalances and metabolic issues. From my own experience, it’s so common to feel stuck with the same old diet and exercise strategies that don’t work because they overlook these crucial factors.
I also appreciate the comprehensive approach that includes mental health support. Weight loss isn’t just physical; addressing emotional eating and motivation is critical for lasting change. This holistic model, coupled with personalized medication like GLP-1 receptor agonists under medical supervision, offers a sustainable pathway rather than quick fixes.
On the practical side, I wonder how others have navigated the challenge of integrating medical prescriptions and personalized nutrition into their daily routines, especially with busy schedules? Moreover, how has ongoing communication with your doctors been managed to successfully adjust your plan when you hit those discouraging plateaus? I’d love to hear how people balance trusting medical expertise while also tuning into their own bodies throughout this complex journey.
What stands out to me in doctor-led fat loss plans is the emphasis on treating weight management as a multifaceted medical issue rather than just a lifestyle choice. This comprehensive approach, especially the use of detailed medical assessments to identify metabolic or hormonal challenges, seems like a huge breakthrough for those stuck in the frustrating cycle of repeated weight loss failures. In particular, the ability to customize medication protocols like GLP-1 receptor agonists and nutritional plans based on an individual’s unique biology feels more promising than the conventional trial-and-error dieting methods.
From what I’ve read and seen, one challenge that might not get enough attention is how accessible and affordable such personalized doctor-led programs are for the average person. While the scientific precision and medical oversight are invaluable, I wonder how many can easily engage in this level of care given potential costs or geographic limitations? It would be interesting to hear from others who’ve navigated this—how did you balance the benefits of personalized medical plans with insurance, affordability, and finding credible practitioners?
Also, the post mentions behavioral and mental health support, which is often overlooked in traditional programs. Integrating psychological assistance alongside medical treatment seems critical, as fat loss is as much a mental journey as a physical one. How have readers found the mental health aspect is addressed in their programs? Has anyone experienced noticeable changes in motivation or emotional eating control after receiving integrated behavioral support?
This post really emphasizes how tailored approaches can make a big difference in weight loss, especially when it involves understanding the hormonal and metabolic intricacies unique to each individual. I personally struggled with stubborn weight gain even after trying various diets and exercise regimes. It was only when I consulted with a specialist who performed detailed metabolic assessments and integrated medication under supervision that I saw meaningful progress. The holistic focus—addressing mental health, hormonal balance, and lifestyle simultaneously—is essential for me because it’s about sustainable change rather than quick fixes. I do wonder, though, how accessible these comprehensive, doctor-led plans are for the average person—are there scalable versions or initial assessments that don’t require extensive investment? Also, how do you sustain motivation when dealing with fluctuations or setbacks, especially in the context of complex biological factors? Would love to hear from others who have navigated these challenging yet promising pathways.
Building on the detailed insights shared in this post, I’ve personally found that the most transformative aspect of doctor-led fat loss plans is their ability to uncover hidden medical issues that often derail conventional methods. Like Jane’s case with hypothyroidism, many of us might be battling unseen hormonal or metabolic challenges that a typical diet would never address. This approach not only personalizes nutrition but also integrates medication when needed, moving beyond mere calorie counting into a medically informed strategy.
From what I’ve experienced and learned from others, one of the real strengths lies in the dynamic nature of these programs. Regular medical assessments allow for tailored adjustments, especially critical when hitting those frustrating plateaus that no amount of willpower or generic advice can overcome. The emphasis on mental health support is also commendable; treating emotional eating and motivation barriers seems essential for sustainable success.
I wonder though, how do people balance trusting medical expertise with listening to their own bodies? Has anyone found effective ways to advocate for themselves in these plans when their personal experiences or struggles seem at odds with standard medical recommendations? It seems like bridging that personal insight with scientific precision is a delicate but important balance in doctor-led fat loss journeys.
I really appreciate how this post highlights the precision involved in doctor-led fat loss plans, especially the emphasis on personalized diagnostics like hormonal profiling and metabolic assessments. It seems that such an approach can unearth hidden factors like insulin resistance or thyroid dysfunction that sabotage traditional diets. From my perspective, one of the most valuable aspects is that these plans don’t just impose a one-size-fits-all regimen but rather adapt dynamically through ongoing medical monitoring. This flexibility is key to overcoming those frustrating plateaus which can otherwise feel like insurmountable barriers.
Regarding the balance between trusting medical expertise and listening to your own body, I think it’s crucial to maintain an open dialogue with your healthcare provider. Personal advocacy can be empowering — for example, if you notice side effects or feel that a particular intervention isn’t aligning with how you feel physically or emotionally, raising these concerns ensures your plan remains truly personalized. Combining scientific guidance with your lived experience seems essential for long-term success.
I’m curious if others have found particular communication strategies or approaches that help them effectively collaborate with their doctors during such complex and evolving weight loss journeys? How do you encourage a partnership where both medical insight and personal observations are valued?
What I find especially compelling about doctor-led fat loss plans is their deep integration of medical diagnostics like metabolic rate assessments and hormonal profiling to create truly personalized strategies. It’s eye-opening to realize how many hidden factors, such as insulin resistance or thyroid issues, can quietly undermine the best efforts when following typical diet and exercise regimens. The tailored incorporation of prescription medications like GLP-1 receptor agonists, under careful physician oversight, adds a level of efficacy and safety seldom found in self-directed programs.
From reading the post and reflecting on my experience, the holistic approach that also addresses the psychological components—like emotional eating and motivation—seems vital for sustained success. Plateaus, for instance, become less frustrating when there’s ongoing monitoring and real-time adjustment in the program rather than a static plan.
I’m curious about others’ experiences with the dynamic nature of these plans: how have you managed the balance between trusting medical guidance and listening closely to your bodily feedback? Also, for those who have utilized advanced pharmacotherapies, how did you integrate those treatments into your daily routine without feeling overwhelmed? It seems like the partnership between patient and doctor is key to making these sophisticated and nuanced plans work effectively over the long term.
What really caught my attention was how doctor-led fat loss plans go far beyond the usual calorie counting and exercise advice by digging into individual medical details like hormonal imbalances and metabolic challenges. This deep dive allows for truly customized strategies, which seems essential given how often weight loss plateaus tend to frustrate us. From what I’ve gathered and somewhat experienced during my own health journey, the ongoing medical supervision and frequent adjustments to medications and diet, guided by lab results and personal feedback, make a huge difference in overcoming those stuck points.
I’ve tried focusing solely on lifestyle changes before but hit walls repeatedly, so having that scientific precision combined with lifestyle tweaks could be the game changer. The emphasis on mental health support also resonates deeply—as emotional eating and motivation swings are huge hurdles for me and many others.
For those who’ve been through or are currently navigating these programs, how do you manage integrating the medical complexities with everyday life routines without feeling overwhelmed? And how proactive have your doctors been in tailoring treatments as new issues or plateaus arise? It’d be great to learn tips on fostering an effective partnership with healthcare providers to keep momentum and stay motivated throughout such a personalized weight loss journey.